In an article he posted online in October 2016, the actor Ben Stiller revealed that he was diagnosed with prostate cancer in 2014.1 He described the positive effects of undergoing prostate-specific antigen (PSA) screening for prostate cancer and discussed the current controversy among experts who debate whether PSA screening is a good idea.
The PSA Screening Controversy
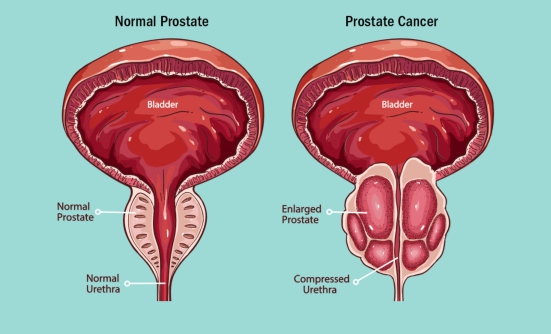
The PSA test measures the levels of a chemical specific to the prostate gland in men. Elevated PSA levels in the blood may indicate that the man has prostate cancer, but high PSA levels can also suggest other potential problems not always related to cancer.
Because of its low level of specificity (that is, inability to zero in on one reason), the PSA test does not differentiate between lethal and nonlethal types of cancer, or even between other medical conditions—such as benign prostatic hyperplasia (or BPH) or early prostate cancer—that are either not related to cancer or show a tumor that is very slow-growing and most likely will not be life-threatening and should not be treated.
This explains why using PSA screening to detect prostate cancer has been associated with too many (and sometimes false) diagnoses of prostate cancer, which can result in overtreatment in men who may not need treatment. This has caused some experts to suggest that PSA screenings may not be a good way to diagnose prostate cancer.
Ben Stiller’s Case
In Stiller’s case, his doctor recommended that he undergo a baseline PSA test at age 46, even though he had no symptoms and had no known risk for this cancer.
“Taking the PSA test saved my life. Literally. That’s why I am writing this now. There has been a lot of controversy over the test in the last few years,”1 Stiller writes. During the next year and a half, his PSA level kept rising, so eventually, his urologist performed a physical exam to determine why.
Based on the physical exam, the urologist ordered an MRI test and then a biopsy, which, to his surprise, showed a Gleason score of 7. A Gleason score helps predict the aggressiveness of prostate cancer. Stiller’s score indicated “mid-range aggressive cancer.”
Stiller was told that the disease was detected early and was treatable. He opted to remove the tumor with a robotic-assisted laparoscopic radical prostatectomy, and no sign of cancer was detectable after that treatment.
Stiller wrote in his blog, “I got diagnosed with prostate cancer Friday, June 13th, 2014. On September 17th of that year, I got a test back telling me I was cancer free. The three months in between were a crazy roller coaster ride with which about 180,000 men a year in America can identify.”1
Second Most Common Cancer in Men, but Experts Disagree about Testing
Prostate cancer is the second most common cancer in men in the United States, after skin cancer; 1 in 7 men in the United States will be diagnosed with this type of cancer in their lifetime. The medical community is not in agreement about whether, or at what age, men should be screened for prostate cancer; instead, men are urged to talk to their doctors about whether and when they should be tested for this disease.
The American Cancer Society and the American Urological Association recommend that PSA testing should begin at age 40 for men who are at high risk; in addition, the American Cancer Society suggests that all men who are not at high risk should begin PSA testing at age 50.
Those who are considered to be at high risk for prostate cancer are African American men and men whose father, brother, or son was diagnosed with prostate cancer at an early age.
“This is a complicated issue, and an evolving one,” Stiller writes. “But in this imperfect world, I believe the best way to determine a course of action for the most treatable, yet deadly cancer, is to detect it early.”1
Advocate for PSA Screening
Because prostate cancer typically has no warning signs or symptoms until it has progressed to the advanced stages, screening may help catch it before it spreads, and when it can still be successfully treated. That was the case for Stiller, who credits his doctor for being proactive.
“If he had waited, as the American Cancer Society recommends until I was 50, I would not have known I had a growing tumor until two years after I got treated,” Stiller writes. “If he had followed the U.S. Preventive Services Task Force guideline, I would have never gotten tested at all, and not have known I had cancer until it was way too late to treat successfully.”1
The Stiller Effect?
Some people have suggested that his disclosure could lead to a so-called Stiller effect on early screenings for prostate cancer, similar to the impact that the actress Angelina Jolie had on genetic testing for breast cancer associated with the BRCA genetic mutation, or the spike in colonoscopies that was attributed to Katie Couric after she had a colonoscopy performed live on the Today Show following her husband’s death from colon cancer in 1998.
But Sean Cavanaugh, MD, Chief of Radiation Oncology at the Cancer Treatment Centers of America near Atlanta, is doubtful. “Sadly, I don’t see this being similar to those examples,” Dr. Cavanaugh says. “Colonoscopy and BRCA testing were recommended screenings that celebrities pushed into the spotlight. Stiller is pushing something that isn’t part of current national guidelines—his viewpoint is deeply opposed by the powers that be. While I wish his story would move the needle on PSA screening, I would be surprised,” he noted.
However, even if Stiller’s disclosure only sparks a conversation between men and their doctors about the optimal time to begin prostate cancer screenings, many people may consider that a success and a contribution to men’s health.
Reference
- Stiller B. The prostate cancer test that saved my life. October 4, 2016. Medium.com. https://medium.com/cancer-moonshot/the-prostate-cancer-test-that-saved-my-life-613feb3f7c00.
This article is based, in part, on a blog prepared by Cancer Treatment Centers of America, with clinical oversight by Maurie Markman, MD.
Key Points
- Prostate cancer is the second most common cancer in men in the United States, after skin cancer
- 1 in 7 men in the United States will be diagnosed with this type of cancer in their lifetime
- The American Cancer Society and the American Urological Association recommend PSA testing at age 40 for men at high risk and at age 50 for other men
- African American men, and men whose father, brother, or son was diagnosed with prostate cancer at an early age are at high risk for prostate cancer
- Because this cancer typically has no warning signs until it has progressed to the advanced stages, screening may help to catch it early when it can still be cured
Patient Resources
American Cancer Society
www.cancer.gov/types/prostate/patient/prostate-treatment-pdq
Centers for Disease Control and Prevention
www.cdc.gov/cancer/dcpc/resources/features/prostatecancer/index.htm
National Cancer Institute
www.cancer.gov/types/prostate/patient/prostate-treatment-pdq