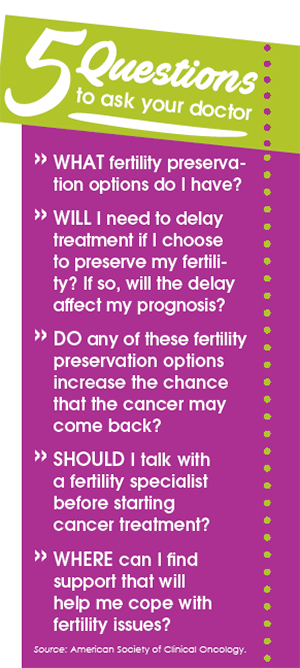
Many young adults with cancer don’t ask questions about their ability to have children after cancer treatment, despite wanting to have biological children. Cancer treatments can affect different organs of the body, including the reproductive organs. Not asking the right questions about fertility preservation before starting chemotherapy, radiation, or other treatments for cancer can lead to fertility problems and even infertility later on.
A new study from the American Cancer Society (published in July 2016 in the journal Cancer) shows that some young women report serious regrets about the impact of cancer treatments on their fertility. With the potential to have such a big impact on their lives, why do many young men and women remain in the dark about undergoing fertility preservation before cancer treatment? The answer is simple: no one is discussing it with them.
Although there are several reasons that young adults don’t undergo fertility preservation before cancer treatment—such as cost, time constraints, and emotional distress—many are not even aware that it’s needed.
Cancer Treatment Can Affect Fertility
The recent study shows that many female cancer survivors aged 18 to 35 years didn’t receive enough information about their risks for infertility and early menopause because of treatment. And more than half of the women felt that their options for fertility preservation were not discussed enough with them before treatment.
For women, cancer treatment can affect fertility by damaging the reproductive organs or hormone-producing organs needed for reproduction. Damage to the ovaries can cause the loss of healthy eggs, which can lead to infertility or early menopause. For men, certain treatments can damage the production of sperm and can limit the sperms’ ability to function. Chemotherapy and radiation therapy (especially around the pelvic area) can affect fertility, as can the surgical removal of reproductive organs (such as the uterus or testicles) because of cancer.
Fertility Preservation Options
The main well-established fertility preservation options include:
- Collecting and freezing unfertilized eggs (oocyte cryopreservation), which can be used later for in-vitro fertilization
- Freezing and preserving the embryo (embryo cryopreservation), which can be used later for in-vitro fertilization
- Ovarian transposition (oophoropexy), which means surgically moving the ovaries to another part of the body that will not be affected by radiation
- Collecting, freezing, and banking sperm for men
New experimental options still being researched include gonadal and ovarian shielding, in which a shield is placed over the pelvic area to reduce exposure to radiation; ovarian transposition, in which the ovaries are moved out of the field of radiation; and for men, removal of testicular tissue, which can be placed back in the body later.
Reproductive and Emotional Concerns
Undergoing fertility counseling before cancer treatment can reduce regrets after treatment; however, counseling alone is not enough. Getting the facts about common fertility misperceptions is a first step for cancer survivors, and getting the support they need is the second.
Survivors need information on dating and discussions related to their fertility status. More than half of the women in the study worried that their partner or future partner would be disappointed if they could not have children.
Young survivors also need information on alternative family building options, such as in-vitro fertilization, which refers to new methods for becoming pregnant for people who are unable to do so on their own. Of the women in the study who were infertile because of cancer treatment, 92% wanted to have children, but 43% felt they did not receive enough information about alternative family planning options.
Patient Resources
American Cancer Society
www.cancer.net/research-and-advocacy/asco-care-and-treatment-recommendations-patients/fertility-preservation
Memorial Sloan Kettering Cancer Center
www.mskcc.org/cancer-care/treatments/symptom-management/sexual-health-fertility/fertility
National Cancer Institute
www.cancer.gov/about-cancer/treatment/research/fertility-preservation