Whether you are a patient with newly diagnosed multiple myeloma, or you are dealing with a disease relapse, navigating the different treatment options available to you is no easy task. Many questions may be running through your head at any given time during your myeloma journey.
As a nurse practitioner who has been involved in the diagnosis and management of patients with multiple myeloma for the past 20 years, some of the questions I am asked include, “How do I know what treatment is best for me, based on the type of multiple myeloma that I have?” or, “How important is it for me to stay on treatment when I feel good, and when my disease is in remission?” To help you and your caregivers answer these questions, we first briefly discuss how we diagnose and monitor multiple myeloma, then examine your role in this journey.
What Is Multiple Myeloma?
Multiple myeloma (sometimes called just “myeloma”) is a cancer of the bone marrow plasma cells. The plasma cells are an important part of our immune system and are critical to protect us from infection, either with or without a multiple myeloma diagnosis. The plasma cell’s job is to make “Y-shaped” proteins (such as IgG, IgA, and IgM) that are meant to protect people from getting sick. In multiple myeloma, the body is overproducing 1 clone of a normal protein that causes a monoclonal “M spike” in the blood. These M-proteins can be spilled out of the body through the urine.1
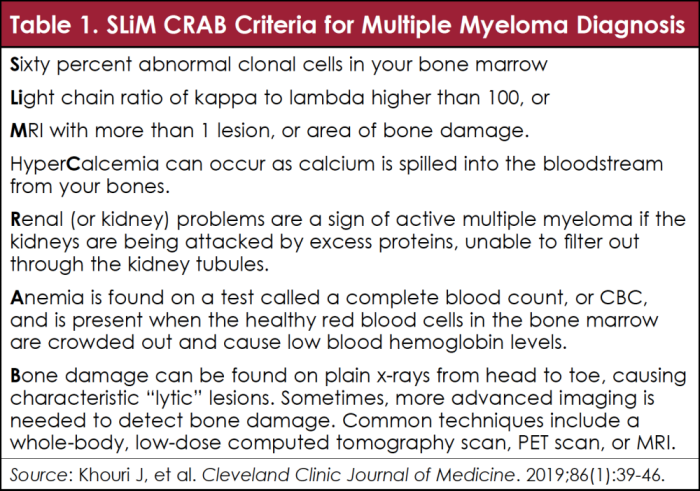
According to the International Myeloma Working Group, patients should be treated for multiple myeloma if they meet “SLiM CRAB” criteria, as outlined in Table 1.2
As you might have read in previous issues of CONQUER magazine, multiple myeloma is not always considered curable, but is very treatable. I have been fortunate to be involved in managing patients in clinical trials that led to the approval of several medications for the treatment of multiple myeloma in the past 2 decades. As a result of clinical trials and the development of effective medications for multiple myeloma, along with improved supportive care with bone strengtheners and antibiotics, patients are living longer than ever and even exceeding a normal life span in some cases.
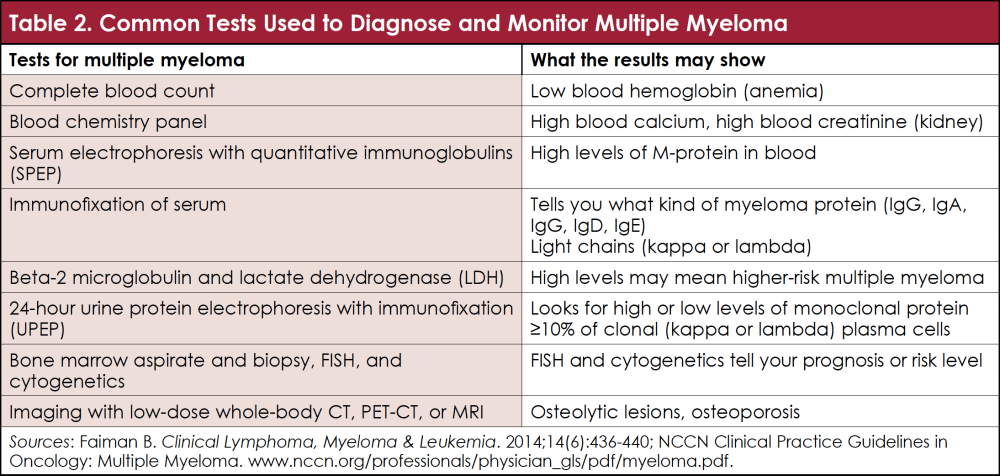
If you or a loved one has multiple myeloma, it is important to find out what type of protein is present in the blood and/or urine, and how high the levels of those proteins were at diagnosis, so that your treatment team can monitor your blood and urine proteins on a regular basis, every month for the first year. I find it very reassuring when patients want to learn about their type of multiple myeloma and monitor their lab results. Depending on your type of multiple myeloma, your healthcare provider may monitor your lab results less often the longer you are in remission. Table 2 lists some common blood tests and what these mean.3,4
A Personalized Approach to Therapy: What Are Your Treatment Goals?
When patients are diagnosed with multiple myeloma, it is easy for healthcare providers to assume that the patients and/or caregivers want the treatment that will give them the best remission and the longest survival. This may be true for some patients, but not for all. So, when patients and caregivers ask what is the best treatment for them, I advise that knowing your personal goals of therapy and the biology of your multiple myeloma can help guide your treatment.
Do you have a high-risk or a low-risk type of multiple myeloma? This is important, because different treatments are often recommended for high-risk patients than for low-risk patients. Although many patients with newly diagnosed multiple myeloma are offered 4 to 6 months of standard treatment to get the disease under control, then undergo a stem-cell transplant using your own cells, followed by a maintenance period, this approach may not be right for you.
Are you working full-time as a single parent, or are you retired but caring for a spouse or a significant other who is ill? By asking yourself what is important to you in your life, you can discuss what treatment is right for you with the members of your healthcare team. Patients with high-risk multiple myeloma may need to take a more aggressive approach to get their disease under control than those with a standard type of multiple myeloma.4
Know Who Is on Your Treatment Team
Whether you receive care in a small community hospital or at a large treatment center, most patients and caregivers have a team of professionals who can help them navigate the many treatment options currently available in the United States. Your care team may consist of a doctor, master’s degree or doctorate-trained advanced practice providers (such as nurse practitioners, nurse specialists, or physician assistants), nurse navigators, social workers, financial counselors, pharmacists, and other subspecialists. Sometimes you may feel more comfortable discussing your treatment options with a trusted nurse navigator or an advanced practice provider than with your doctor.
Concerns about the type and cost of treatment can be addressed by anyone on your team. Most team members are capable of finding at least some financial assistance so that you could receive the right treatment for you, whether the treatment is given as an oral medication, as an injection, or intravenously, and administered either close to home or at a larger treatment center.
It is also important to consider clinical trial participation. Clinical trials further test new medications and therapies. The protocols of these clinical trials adhere to accepted standards of patient safety, and patients must be provided informed consent. As of 2021, many well-designed clinical trials are available that offer patients standard treatments as well as the possibility of a newer and better treatment. In addition, when participating in clinical trials you often have a dedicated research nurse, study staff, and other benefits. Parking and travel reimbursement are often just a few benefits that patients can enjoy, which offset the costs of care.
Some of your goals of treatment may also be to help other patients through the advancement of science, to learn better ways to give the medicines we have, or discover new and improved medications. If you are not offered the option of joining a clinical trial at diagnosis or throughout your multiple myeloma journey, don’t forget to ask if there are any available to you.
What Is My Role in Achieving My Desired Outcomes?
Patients have many ways they can participate in their multiple myeloma journey. Adherence, or the ability to continue treatment as recommended by your healthcare providers, is critical to your success. But just because your doctor or healthcare provider recommends a specific treatment doesn’t mean that you have to take it. In my practice, we involve the patient, caregiver, and healthcare team to make treatment decisions together through a process called “shared decision-making.”
Studies have shown that you are more likely to take treatment as recommended if you believe that the treatment is right for you. Speak with your doctors, nurses, and other care team members about all your options, because many treatment options are available for most patients.5,6
Most providers recommend that patients continue their treatment even if their disease is in remission. This is because multiple myeloma is a clonal bone marrow disorder. Think of your bone marrow as a garden. Myeloma cells are like the weeds in your garden. Although we can test your blood, urine, and even your bone marrow to determine how deep your disease remission is, these myeloma cells, or weeds, can grow back over time, even if we think that they have disappeared.
The current standard of care outside of a clinical trial is to offer continuous treatment to patients to suppress the myeloma cells and their precursors and prevent them from growing back. That is, unless you are having significant side effects from the treatment, or if your multiple myeloma returns. Talk to your healthcare provider about what is right for you, and make a list of questions ahead of your appointments to ask your treatment team when deciding what therapy is right for you, and how long to continue the treatment.
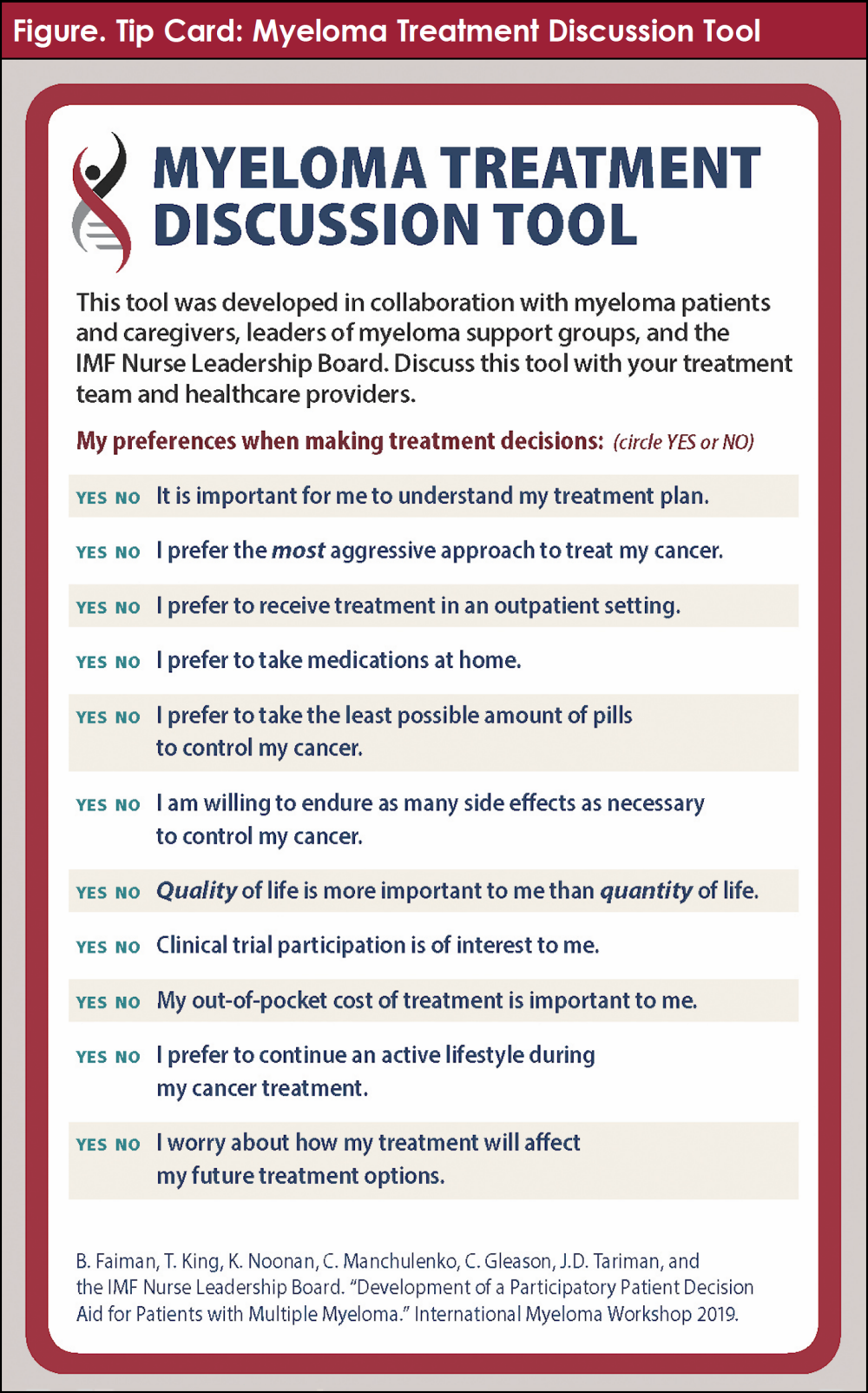
To facilitate a discussion between you and the members of your care team in your specific situation, consider using the Tip Card from the International Myeloma Foundation provided in the Figure. This 4-page tool (available at https://imf-d8-prod.s3.us-west-1.wasabisys.com/2021-04/TC-Patient-Tool-EN-2021.pdf) can help you prepare your questions to determine what you and your team agree is the best treatment for you.7
A Few Words of Wisdom
Each treatment regimen carries risks, benefits, and certain side effects. Addressing these side effects and monitoring your disease requires guidance from your care team to manage these symptoms. Be an active participant in your care. Ask questions about your disease status (high or low risk), monthly lab values, any side effects you may have or are having from the treatment, and how to manage any side effects.
Finding out who is on your care team, and who to call if you have any questions or concerns regarding your care, can facilitate communication. You are your best advocate, and know what is best for you and your caregiver.
In addition, if your treatment is too expensive, and you are struggling financially, please speak up. Do not suddenly stop treatment for any reason before you have a discussion with your team. Finally, many resources for financial assistance exist, but these resources are often not used. Your social workers, nurses, and other members on your team can help you find support.
References
- Khouri J, Samaras C, Valent J, et al. Monoclonal gammopathy of undetermined significance: a primary care guide. Cleveland Clinic Journal of Medicine. 2019;86(1):39-46.
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncology. 2014;15(12):e538-e548.
- Faiman B. Myeloma genetics and genomics: practice implications and future directions. Clinical Lymphoma, Myeloma & Leukemia. 2014;14(6):436-440.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Multiple Myeloma. Version 3.2022. October 27, 2021. www.nccn.org/professionals/physician_gls/pdf/myeloma.pdf.
- Faiman B. Disease and symptom care: a focus on specific needs of patients with multiple myeloma. Clinical Journal of Oncology Nursing. 2017;21(5 suppl):3-6.
- Faiman B, Tariman JD. Shared decision making: improving patient outcomes by understanding the benefits of and barriers to effective communication. Clinical Journal of Oncology Nursing. 2019;23(5):540-542.
- Faiman B, King T, Noonan K, et al; IMF Nurse Leadership Board. Myeloma treatment discussion tool. 2019. https://imf-d8-prod.s3.us-west-1.wasabisys.com/2021-04/TC-Patient-Tool-EN-2021.pdf.