Atreatment pioneered in the 1890s—at a time when doctors were using sarsaparilla as a blood purifier and gasoline to treat lice infestations—is now making a roaring comeback in oncology. Immunotherapy, or harnessing the body’s immune system to combat disease, has breathed new life into the way doctors treat cancer today. This kind of treatment can specifically and sensitively eliminate the threat of cancer.
More than a century ago, immunotherapy was a burgeoning theory as a way to treat cancer, but it ultimately gave way to radiation therapy and chemotherapy, which were developed in the early and the middle of the twentieth-century, respectively, as more viable medical options.
Why Immunotherapy?
As radiation and chemotherapy became the heavyweights in cancer therapy, patients were no longer boxed into a corner—many have survived their diagnoses. Despite the improvement in survival, however, not all is rosy with those astringent therapies.
Oncologists are still grappling with how to deal with cancer that is refractory (not responding to treatment), recurrent (coming back), and metastatic (spreading).
Oncology doctors are also in a quagmire about the gap in survival for adolescents and young adults (AYAs) with cancer: despite new therapies, the survival rates for patients between ages 15 and 39 have not improved in 30 years. And those who do survive through treatment are often saddled with long-term and serious side effects, for which medicine has yet to find a good answer.
Enter immunotherapy, stage left. This bright star has gained some traction over the past 2 decades, with the promise of more effective and less hazardous ways to combat cancer than the treatments that were dominant in the last century.
Immunotherapy is part of the focus of the National Cancer Moonshot Initiative, whose goal is to find molecular-, cell-, and vaccine-based immunotherapies against cancer; I serve on the Blue Ribbon Panel Working Group for Cancer Immunotherapy and Prevention, and I recently discussed this topic at the 2017 Teen Cancer America 2nd Global AYA Cancer Congress.
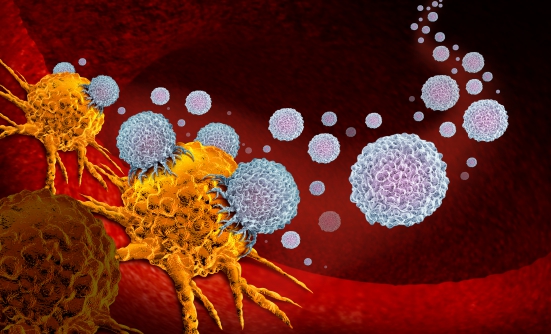
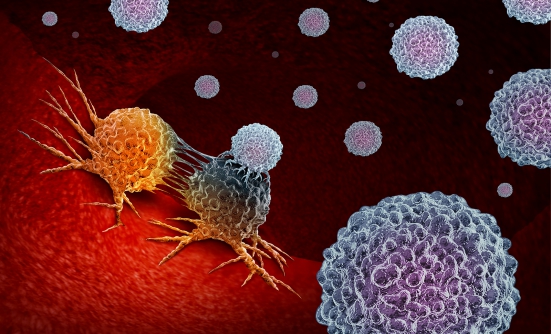
Immunotherapy approaches are powerful, adaptable, durable, targeted, and synergistic. The immune system is constantly on the prowl for foreign invaders, and routinely kills harmful bacteria, viruses, and some cancers in their early stages.
But cancer can give the immune system the slip, by making its cells invisible to the antibodies and T-cells and NK-cells whose job it is to find them.
The 5 Types
By tapping into the body’s cells and organ systems that fight disease, immunotherapy can either generally stimulate the immune system, or specifically help it target cancer cells. Scientists are just now scratching the surface in the development of these interventions, with the current 5 specific types.
- Adoptive T-Cell Transfer (CAR T-Cell Therapy)
This process is akin to bulking up a skinny kid at the gym. Doctors take millions of scrawny and ineffective T- or NK (immune)-cells out of the patient and introduce new genes into those cells, using lenti- or retroviruses, such as a disabled and non-disease-causing form of HIV-like virus, which energize the immune cells’ functionality and number. The patient then receives those engineered immune cells back. If all goes well, those newly equipped and specifically trained immune cells multiply, flex their muscles, and destroy the cancer cells.
- Cancer Vaccines
You can’t start a fire without a spark, and your immune system can’t kill cancer cells without an activator or a vaccine. Instead of taking cells from the body, doctors inject a patient with a vaccine—in the form of dead cancerous cells, nanoparticles, DNA vaccines, or professional antigen-presenting cells. The body then incubates the vaccine: if it takes hold, the vaccine prompts an immune reaction, educating and deploying the immune cells to attack the invading cancer.
- Monoclonal Antibodies
Imagine putting up a giant flashing neon sign that says, “The cancer is here!” That’s the case with monoclonal antibodies. Antibodies are molecules that flag proteins in the body as invasive, cueing the immune system to attack them; with cancer, it’s certain types of proteins called antigens.
Monoclonal antibodies can work on their own, by unleashing the immune system’s power, or in combination with chemotherapy or radiation, for added potency.
- Immune Checkpoint Blockade
A healthy immune system knows the difference between an invading organism, such as bacteria or virus, and its own cells. To tell the difference, the body’s own cells have molecular brakes called “checkpoints,” which stop the body from destroying itself.
A master chameleon, cancer will turn those checkpoints on to go undetected. Doctors use checkpoint inhibitors that disable cancer’s invisibility shield, allowing the immune system to do its job.
- Manipulating the Tumor’s Microenvironment
Not every cell within a tumor is cancerous. For instance, there are cells that provide protection for the growing tumor and can be targeted with specific therapies.
Challenges
Immunotherapy is increasingly used to treat cancer, but it has some drawbacks. Not all cancer facilities can provide adoptive T-cell therapy, and it can also be too expensive for some patients. In addition, many of the immunotherapies available today don’t specifically help young patients.
Still, I am encouraged by the promise of this approach. Immunotherapy today is a viable alternative, and a complement to traditional treatments. We’ve made great strides already, and we’ll continue to make progress as we develop more therapies. Immunotherapy is well on its way to become the backbone of future cancer treatment.
Key Points
- Oncologists are still grappling with how to deal with refractory, recurrent, or metastatic cancer, creating an opportunity for immunotherapy
- The 5 types of immunotherapy are adoptive T-cell transfer, cancer vaccines, monoclonal antibodies, immune checkpoint blockade, and manipulating the tumor’s microenvironment
- The drawbacks of immunotherapy are that not all facilities are able to provide adoptive T-cell therapy, and it can be a very expensive option