You’ve been diagnosed with multiple myeloma, and your oncologist suggests you get a transplant. Or perhaps your cancer relapsed and a transplant is proposed. Your doctor may use the term “stem-cell transplant” (SCT for short) or “autologous” (auto for short) transplant as a treatment option. Transplants for newly diagnosed patients typically fit within a treatment scheme that includes induction SCT, then maybe consolidation therapy, and then possibly maintenance treatment.
We will assume you are a transplant-eligible patient with multiple myeloma; however, transplant eligibility is one of the first things a doctor considers when determining the course of treatment. Although “chronological age,” typically less than 70 to 75 years, plays an important factor in transplant eligibility, so does your “physical age” and overall well-being. That is, the doctor will consider if the patient has other health issues, such as heart problems, as well as the availability of a care partner who could play an important role in supportive care during transplant and recovery.
You may first ask, “What exactly is being transplanted?” At least, that was my first question, because a transplant for multiple myeloma is not similar to a heart or a liver transplant; meaning that the patient is not receiving a new organ. As we’ll see, it’s all about the immune system.
What Is Stem-Cell Transplant?
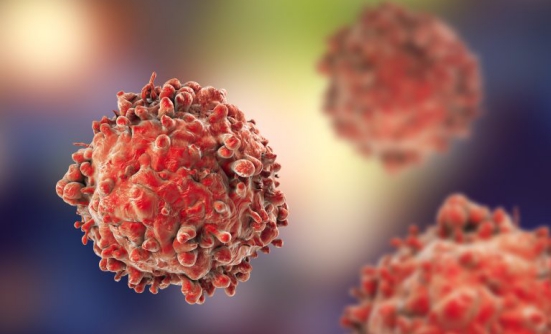
So let’s consider the SCT procedure. A transplant begins with induction therapy, which is typically 4 to 6 cycles of drugs for multiple myeloma, such as Revlimid (lenalidomide), Velcade (bortezomib), and dexamethasone, to reduce the myeloma cells as much as possible.
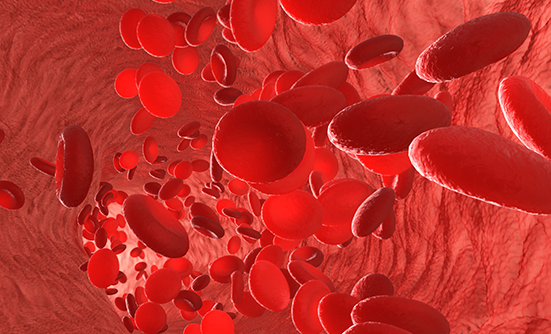
Next comes a procedure called “apheresis,” in which stem cells that normally reside in your bone marrow are collected (or “harvested”). Because the apheresis machine cycles your blood, you’ll receive injections of G-CSF (or granulocyte colony-stimulating factor), which encourage your body to make more stem cells and move them from the bone marrow into the bloodstream for easier collection of the stem cells. You may also get other medications to help this “mobilization” procedure. Our stem cells produce our blood cells (red, white, and platelets) and build our immune system.
Depending on the treatment facility, you may also have a catheter to enable easier access to apheresis instead of IV lines. After a few days, you’ll be connected to the apheresis machine, which circulates your blood, collects stem cells, and returns your remaining blood. Typically, enough stem cells are collected for 2 transplants, taking 2 to 4 sessions of 3 to 4 hours. Although the G-CSF shots can cause bone pain, side effects from apheresis are usually minimal, so bring a good book or a movie. Your stem cells are then frozen for future transplants.
Your transplant begins a few weeks later, with very high-dose chemotherapy, usually using the chemotherapy drug melphalan. The goal is to kill whatever myeloma cells remain in your body, but this also kills your healthy stem cells, and, thus, your blood cell count and immune system are greatly compromised. Within 2 days, you receive back your previously harvested stem cells over 20 minutes in a somewhat “anticlimactic” infusion. This is considered a “rescue procedure”—enabling these stem cells allows you to rebuild your blood cell counts and your immune system. Each day, your blood will be drawn and analyzed to determine when your blood cell counts start to recover.
You’ll also hear the term “neutropenic,” meaning that your white blood cell count is less than 1.0, indicating that your immune system is very low. During this period, it’s important to avoid any infection. You are probably not feeling too well physically, you may be nauseous, very tired, and experiencing painful mouth sores. Although treatments are available for these side effects, you’ll physically feel much better perhaps 10 to 12 days later, when your white blood cell count is above 1.0, and all your other blood cell counts continue to improve.
Your Initial Care
The transplant procedure typically takes about 3 weeks, and cancer centers will perform an SCT in the hospital or in an outpatient setting. Inpatient means that you stay in the hospital for about 3 weeks. Outpatient procedure means that you may only be in the hospital for 1 to 2 days, and the rest of the time you can be outside of the hospital. However, you’ll still need to report to the center daily for blood draws, and you should also be nearby if you have a temperature spike.
Your care partner will be of tremendous help, monitoring your temperature, cleaning your catheter, and driving you to your daily appointments. You’ll continue to be monitored closely after your blood cell counts and immune system recover, and you’ll still need to minimize your risk of infection.
You may experience fatigue for weeks or months post-transplant. Of course, the goal of the SCT is to reduce your measurable myeloma cells to zero, but that doesn’t always happen. As such, your doctor may suggest that you seek additional treatment, especially maintenance treatment, to keep the multiple myeloma from returning for as long as possible.
Types of Transplants
There are several types of transplants that your doctor may discuss with you. Tandem transplant involves 2 SCTs, with the first SCT followed by a second SCT within 2 to 4 months. This procedure was pioneered at the University of Arkansas and is still used at some centers. Are 2 transplants better than 1? The evidence is not sufficient to say Yes or No.
In addition to auto SCT, allogeneic (or “allo”) transplant is similar to auto SCT described above, with one very important exception. In allo transplant, the stem cells are collected from a donor rather than from the patient, and your immune system is replaced with a new immune system created by those donor stem cells. You may hear doctors describing the allo transplant as a potential for a myeloma cure, because the new immune system may well be able to kill any remaining myeloma cells in your body.
Donor Stem Cells
Donor stem cells can come from siblings, other family members, unrelated adult donors, or even umbilical cords. However, this new immune system will likely cause graft-versus-host disease (GVHD), which can cause skin, liver, or intestinal problems, because the job of the immune system is to eradicate any foreign elements from your body. Just as your new immune system may do a great job in eliminating myeloma cells, it may also want to eliminate other body organs, such as your kidneys, liver, and skin, all of which appear foreign to this new immune system.
And although new drugs can suppress GVHD, you don’t want to suppress its helpful graft-versus-myeloma effect, which presents a catch-22. To minimize GVHD, doctors will look for the highest possible donor compatibility, by trying to match the immune system markers between you and the donor. But because a blood type is not one of those markers, a patient with multiple myeloma can end up with a different blood type. A sibling has a 1 in 4 chance of being a donor match, but from there the odds go down significantly, generally requiring donor searches via large bank-matching services, such as BeTheMatch.
Recovery Period
The recovery time frame for an allo transplant for multiple myeloma is long and difficult. A patient may be hospitalized for 2 months, followed by daily blood draws to manage the GVHD. Because complications often arise, allo transplant in multiple myeloma has a high, 35% to 45% mortality rate compared with less than 1% for auto transplants. Therefore, allo transplant is no longer used much in multiple myeloma, although it is sometimes considered for younger patients.
To reduce this high death rate, a version of an allo transplant called a reduced-intensityconditioning transplant (also called “non-myeloablative” or “mini” transplant) was developed in the late 1990s that involved little or no upfront chemotherapy and slowly introduced donor stem cells to create a new immune system.
This procedure typically involved 2 transplants—an auto SCT followed by a mini-allo. Although the mortality rate was reduced to about 15%, it still was not better than a single auto transplant. And with so many new multiple myeloma treatments available today, even 15% is a high mortality rate if the procedure doesn’t improve patient outcomes.
The Future of Transplant?
Although auto transplant used to be considered the “gold standard” of treatment for patients in the past decades, opinions vary today. Some doctors still consider it the preferred treatment, but other doctors suggest that it is only one of many possible treatments.
The use of transplant may also depend on the patient’s risk level, with doctors favoring its use for high-risk patients, and on the patient’s objectives, who may choose not to have an SCT because of the long time away from work.
Patients with multiple myeloma need to get as much expert advice from multiple myeloma doctors, including second opinions, for all treatments to make an educated decision that’s best for the individual patient.