Evidence shows that lack of health insurance in the United States can determine survival of patients with cancer. Experts have debated whether racial (or ethnic) disparities in the care patients receive affect their outcomes, with some suggesting that the differences relate to biological or socioeconomic differences rather than the treatment that different ethnic groups receive. Although different races have different risks for specific types of cancer, clearly the quality of cancer care should be the same for all patients, regardless of who they are or where they live.
A new study presented at the 2019 meeting of the American Society of Clinical Oncology (ASCO) shows that the explanation is rather simple—limited access to cancer care, mostly for lack of health insurance or insufficient coverage—accounts for most of the disparity seen between black and white patients with cancer.1
According to this study, states that expanded their Medicaid program (for people without insurance) under the ACA (or Obamacare) practically eliminated racial differences in cancer and outcomes.1
Health Insurance Improves Outcomes
For people facing cancer, it surely is not surprising to learn that their chance of better outcomes and possibly even survival increases by having health insurance, considering the high, and often astronomical, cost of cancer therapies today.
Richard L. Schilsky, MD, FACP, FSCT, FASCO, Senior Vice President and Chief Medical Officer of ASCO, agreed. “If you can’t access care, you can’t benefit from care. For all the advances we’ve observed in recent years in cancer treatment, in cancer care broadly speaking, if you don’t have insurance, if you can’t access care, if you can’t get care in a timely fashion, you can’t benefit,” Dr Schilsky said at the ASCO meeting.
The researchers of that study examined data of people (aged 18-64 years) who received treatment at 800 cancer centers in the United States, including community cancer centers and academic medical centers. The study included patients with advanced or metastatic solid tumors (including lung, breast, prostate, urothelial, gastroesophageal, colorectal, renal-cell cancer, and melanoma).
Medicaid Expansion Eliminates Care Disparities
The researchers reviewed the data of 18,678 patients who received cancer treatment in 33 states before they expanded their Medicaid program under the ACA, and in states that chose not to expand their Medicaid program, and compared them with 11,708 patients who received cancer treatment in states that did expand Medicaid.
Among patients who received treatment in states without or before a Medicaid expansion, 48.3% white patients received systemic therapy within 30 days of their cancer diagnosis versus only 43.5% of black patients—almost 5% more white patients than black patients receiving timely care.
However, in states where Medicaid was expanded, this difference in timely care was almost completely erased between black and white people. Timely treatment is especially important in cancer, when delaying care can mean the difference between life and death.
“This study extends prior evidence regarding the effect of the ACA and tells us that national healthcare coverage policies may reduce disparities,” said Amy Davidoff, PhD, MS, Senior Research Scientist in Public Health, Yale School of Public Health, New Haven, CT, and lead author of the study.
“This work is to be commended. This is some of the best evidence we have to date that policies can impact outcome, particularly timely treatment. Everyone benefits and has some level of improvement,” said William Dale, MD, PhD, Arthur M. Coppola Family Chair in Supportive Care Medicine, City of Hope, Duarte, CA.
“People falling behind before they had access to care, and disparity disappeared after Medicaid expansion,” Dr. Dale said.
The ACA Improved Ovarian Cancer Diagnosis

A separate study also presented at the meeting showed that the ACA led to a substantial increase in the diagnosis of early-stage (stages I and II) ovarian cancer in women.2
“More than 22,000 women will be diagnosed with ovarian cancer this year, and half will be dead in 5 years. We have no screening methods for detection, and by the time patients are symptomatic, the disease is diagnosed at an advanced stage,” explained Anna Jo Smith, MD, MPH, MSc, Resident, Department of Gynecology and Obstetrics, Johns Hopkins University, Baltimore, and lead author of the study.
“The implication of our study is that under the ACA, women with ovarian cancer are more likely to be diagnosed and receive early treatment. These gains may have a long-term impact on survival, health, and well-being for women diagnosed with ovarian cancer,” Dr. Smith said.
“This study shows that access to healthcare can eliminate disparities and increase access to earlier diagnosis and earlier treatment, and ultimately improve long-term outcomes for patients with ovarian cancer,” agreed Merry Jennifer Markham, MD, FACP, of the University of Florida Health Cancer Center, Gainesville.
A Black Woman with Breast Cancer
A recent article described the case of Ms. M., a black woman with breast cancer, highlighting how structural racism (social structures and institutions) can lead to unequal care and influence cancer treatment in areas with a high minority population.3
Ms. M. is a 60-year-old, uninsured black woman who found a lump in her breast and went to the emergency department (or ER) in her black neighborhood in the South Side of Chicago. The ER doctor said this was an infection and prescribed antibiotics, without doing tests to find the cause of the lump.
When her lump did not clear with antibiotics, Ms. M. had a mammogram, which showed she had breast cancer. She received no more information about it and was referred to a general surgeon—instead of a cancer specialist—who wanted to do a mastectomy (removal of the breast).
Luckily, Ms. M. was contacted by a patient navigator, who was sent by the Metropolitan Chicago Breast Cancer Task Force, which was founded in 2008 to reduce disparities in breast cancer mortality between black and white women. The Task Force had found that black women were nearly 40% less likely than white women to receive good breast care, which may explain the high likelihood of a missed diagnosis of breast cancer on a screening mammogram among black women.
The navigator referred Ms. M. to a surgical oncologist at an academic center who provided appropriate care for her.
Ms. M.’s experience highlights the obstacles to appropriate care related to racial inequalities. In Chicago, hospitals located in minority neighborhoods have lower performance scores related to cancer care.
The authors of this article noted that although breast cancer mortality among white women in Chicago and across the country have dropped with improved screening and new treatments, these rates did not improve as much among black women.
Cancer Disparities
According to the National Cancer Institute, in the United States:
- Blacks are more likely to die of many types of cancer than any other ethnic group
- Black women are much more likely than white women to die of breast cancer, and this gap is increasing; they are more likely than any other group to die of cervical cancer
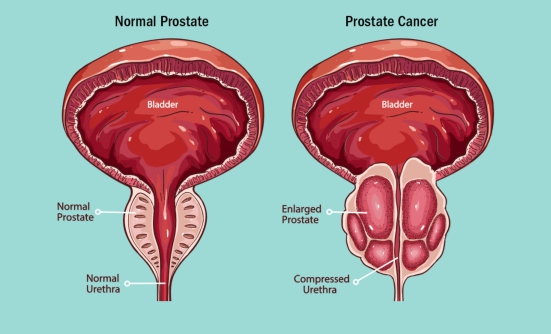
- Black men are more than twice as likely than white men to die of prostate cancer, and nearly twice as likely to die of stomach cancer and of multiple myeloma
- Black men are more likely to have and to die of lung cancer than any other ethnic group
- American Indians and Alaska Natives are more likely to die of kidney cancer, followed by Asian and Pacific Islanders
- American Indians and Alaska Natives are more likely to be diagnosed with liver cancer than any other racial group
References
- Adamson BJS, Cohen AB, Estevez M, et al. Affordable Care Act (ACA) Medicaid expansion impact on racial disparities in time to cancer treatment. Journal of Clinical Oncology. 2019;37(suppl):Abstract LBA1.
- Smith AJ, Nickels A. Impact of the Affordable Care Act on early-stage diagnosis and treatment for women with ovarian cancer. Journal of Clinical Oncology. 2019;37(suppl):Abstract LBA5563.
- Pallok K, De Maio F, Ansell DA. Structural racism—a 60-year-old black woman with breast cancer. New England Journal of Medicine. 2019;380 (16):1489-1493.
Key Points
- New evidence confirms the role of health insurance in determining the quality of cancer care
- Medicaid expansion virtually erased treatment disparities between white and black people with advanced or metastatic cancer
- In states that did not expand Medicaid, racial disparities persisted among patients with cancer
- The case of a black woman with breast cancer and no insurance highlights racial disparities in cancer care
Patient Resources
Centers for Disease Control and Prevention
www.cdc.gov/cancer/healthdisparities/index.htm
National Cancer Institute
www.cancer.gov/about-cancer/understanding/disparities