Increased focus on racial disparities in cancer care in the past few years has shown a link between unequal access to best available care and poor clinical outcomes for patients with cancer from minority populations. A new study presented at the 2021 ASCO Annual Meeting showed that improving prostate cancer screening for black men can improve outcomes and save lives.
Racial Disparities
Overall, black men are diagnosed with prostate cancer at a younger age and with a more advanced stage of cancer than white men, and they are therefore more likely to die from prostate cancer than white men.
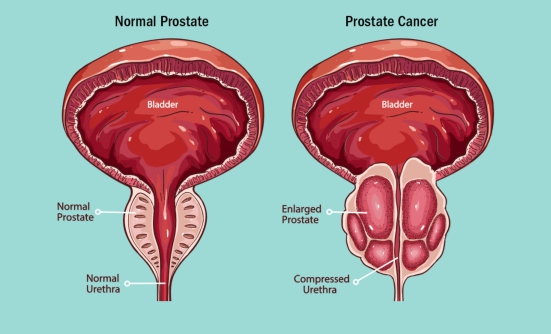
An analysis of nearly 4,700 black men diagnosed with prostate cancer at the Department of Veterans Affairs (VA) over a 13-year period has shown that increasing the rates of prostate-specific antigen (PSA) screening (used to diagnose prostate cancer) reduces the risk of late diagnosis of prostate cancer, when the cancer is at an advanced stage or when it has already metastasized (spread to other organs). As in all types of cancer, early diagnosis with PSA screening can reduce the death rates from prostate cancer.
These results suggest that increasing PSA screening in men will lower death rates from prostate cancer, the researchers concluded.
“Our study is just one step in addressing the racial disparities that still exist in prostate cancer and prostate cancer screening,” said Edmund M. Qiao, BS, Medical Student in the Department of Radiation Medicine at the University of California San Diego in La Jolla, California.
“Access to care barriers disproportionately affect African-American men, and this is driven by issues such as insurance status, screening availability, and treatment choices,” he emphasized.
Because black men are diagnosed with prostate cancer at a relatively young age and with an advanced cancer, their risk of dying from prostate cancer is greater than that of white men with prostate cancer. Despite these disparities, fewer black men than white men are included in prostate cancer clinical trials. In fact, the 2 clinical trials on which the current national PSA screening guidelines are based enrolled no black men under age 55.
“More research is needed to address all of the existing racial disparities within prostate cancer,” Mr. Qiao added.
Study Population
For this study, Mr. Qiao and colleagues used data from the VA to study the effect of PSA screening in 4,654 black men aged 40 to 55 (a relatively young age for prostate cancer) who were diagnosed with prostate cancer between 2004 and 2017.
The researchers analyzed the stage of cancer at diagnosis by using several factors normally used to diagnose prostate cancer, including the PSA test results, the Gleason score, and whether it was metastatic cancer at diagnosis. They also analyzed the rate of death from prostate cancer.
Patients were divided into 2 groups by high and low rates of PSA screening. On average, patients in the high PSA-screening group had 3 previous PSA tests. By contrast, the average for the men in the low PSA-screening group was less than 1 (0.5) previous PSA test.
Fewer PSA Screenings Linked to Worse Outcomes
An unadjusted analysis showed that the men who had higher rates of PSA screening were generally older, were diagnosed in later years, and had less aggressive tumors at diagnosis, showing the benefits of regular PSA screening.
“After stratifying patients into low and high PSA-screening cohorts, we saw that patients with higher rates of PSA screening had lower severity of disease for all 3 end points: PSA, Gleason score, and metastatic disease,” said Mr. Qiao.
The cumulative rate of death from prostate cancer was also associated with the rates of PSA screening. The rate of death from prostate cancer was about 4% in patients in the low PSA-screening group, compared with a mortality rate of 2% in those with a high rate of PSA screening. In addition, the difference between these 2 groups continued to grow over time.
“At 10 years, patients in the low PSA group had a 6% cumulative incidence of prostate cancer-specific mortality versus 3% in the high group,” Mr. Qiao said.
Finally, results of the multivariable regression analysis showed that PSA screening significantly reduced the risk of advanced or metastatic prostate cancer by about 20% to 40%. PSA screening also reduced the risk of death from prostate cancer by about a quarter (25%).
Key Points
- Overall, black men are diagnosed with prostate cancer at a younger age and with a more advanced stage of cancer than white men
- Black men have a higher risk of dying from prostate cancer than white men
- Fewer black men are included in prostate cancer clinical trials than white men
- Barriers to access to care disproportionately affect black men, which is caused by lack of health insurance, no access to screening, and treatment choice
- Increasing the rates of prostate-specific antigen (PSA) screening (used to diagnose prostate cancer) reduces the risk of late diagnosis and subsequently death
- In one analysis, PSA screening significantly reduced the risk of advanced or metastatic prostate cancer by about 20% to 40%
- PSA screening also reduced the risk of death from prostate cancer by about 25%