By now, virtually everyone living with cancer has heard that immunotherapy is revolutionizing treatment. Immunotherapy, in its various forms, harnesses the body’s own immune system to attack cancer cells. Several types of immunotherapy drugs have already been approved for different types of cancer, such as melanoma, lung cancer (specifically non–small-cell lung cancer), bladder and kidney cancer, and a few types of blood cancers.
Many patients with cancer once believed to have a clear death sentence are now alive years after treatment thanks to these new drugs and new immuno-oncology therapies.
What about multiple myeloma? Do persons battling this rare type of blood cancer have a shot at these impressive new treatments?
“We are continuing to learn about the ways the immune system interacts with different types of cancer, including multiple myeloma,” said Richard Pazdur, MD, Director of the FDA’s Oncology Center of Excellence, in an interview with CONQUER magazine.
What patients with multiple myeloma and many other people may not realize, Dr. Pazdur said, is that 2 drugs that were recently approved for this type of blood cancer are also immunotherapies. Many people have been focused on “checkpoint inhibitors” as the main immunotherapy drugs, but other types of drugs use the body’s immune cells to fight cancer.
New Monoclonal Antibodies for Multiple Myeloma
At the end of 2015, 2 new immunotherapies were approved for patients with multiple myeloma—the “immunostimulatory” monoclonal antibodies that stimulate immune factors to combat and destroy myeloma cells. These 2 immunotherapies are Darzalex (daratumumab) and Empliciti (elotuzumab).
According to multiple myeloma experts such as Paul Richardson, MD, of Dana-Farber Cancer Center in Boston, the monoclonal antibodies work in patients whose multiple myeloma does not respond (or stops responding) to all other approved therapies for multiple myeloma.
“These are paradigm-changing agents,” Dr. Richardson said about these new monoclonal antibodies at last year’s annual meeting of the American Hematology Association (ASH).
Darzalex and Empliciti are often combined with other cancer drugs for multiple myeloma—including the immunomodulator Revlimid (lenalidomide), the proteasome inhibitor Velcade (bortezomib), and dexamethasone (a steroid)—in patients whose disease progressed while using other therapies.
In clinical trials, regimens containing these new drugs have reduced the risk of disease progression or death significantly compared with traditional regimens used without the monoclonal antibodies.
“The introduction of monoclonal antibodies is the most exciting development in recent years,” according to another multiple myeloma expert, Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Minnesota, who also spoke at the 2016 ASH meeting.
Dr. Kumar said that a number of clinical trials are evaluating the addition of Darzalex to other regimens, aiming for even better outcomes. “This will be the path forward,” he said.
Other strategies for stimulating an immune response are also very promising. These include the very innovative CAR T-cell therapy, and anti-PD-1 or anti-PD-L1 monoclonal antibodies, which are better known as checkpoint inhibitors.
CAR T-cell therapy has made headlines in the treatment of certain leukemias, and anti-PD-1 or anti-PD-L1 antibodies have been life-changing in several solid tumors (such as melanoma and lung cancer) and in Hodgkin lymphoma.
In myeloma, these experimental therapies are only available in clinical trials, primarily in patients whose disease is progressing despite the use of several types of therapies.
CAR T-Cell Therapy in Multiple Myeloma
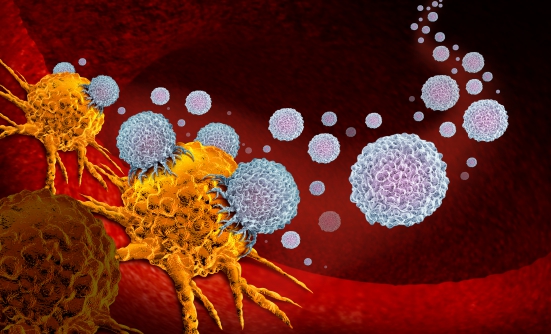
CAR T-cell therapy works through “engineering” to fight cancer. An antigen is a molecule whose shape can be recognized by the immune system. By latching onto an antigen on a cancer cell (like a key in a lock), a T-cell initiates its attack against its target. CAR T-cells are engineered by researchers to become hearty cancer fighters. They are created in a laboratory from T-cells that are collected from the patient, modified to recognize an antigen-binding site on a tumor, then re-infused into the patient. These “programmed” T-cells then expand and persist indefinitely in the body. As “live” cells, they can continue to destroy any cell that displays the target antigen.
James Kochenderfer, MD, of the National Cancer Institute, is leading a pivotal study of CAR T-cell therapy in multiple myeloma. Although this approach should work, Dr. Kochenderfer predicted, there are challenges unique to multiple myeloma that must be overcome before they can be used in patients. These challenges largely pertain to identifying the right antigen to target in this blood cancer.
In a lecture at the 2016 ASH meeting, Dr. Kochenderfer advocated the development of a CAR T-cell drug that will target B-cell maturation antigen (BCMA), which is expressed most uniformly on myeloma cells and not on normal blood cells. According to Dr. Kochenderfer, this is likely to be a winning strategy.
In a small clinical trial of 12 patients with worsening multiple myeloma that expressed BCMA, all patients responded to anti-BCMA CAR T-cell treatment or achieved stable disease, Dr. Kochenderfer reported at the ASH meeting. Other CAR T-cell drugs are also being evaluated in clinical trials, including one known as BB2121, and another that targets the CD19 antigen, which researchers think could prolong the remission of multiple myeloma after a stem-cell transplant.
The trade-off is the potential for some unique—sometimes life-threatening—side effects, as seen in clinical trials with CAR T-cell therapies for leukemia. The robust immune response that is generated in the body can result in a syndrome that includes symptoms similar to severe infection, including very high fevers. Patients can also have temporary, though disturbing, cognitive side effects. However, with proper treatment, these side effects typically resolve over the course of a few days.
“We are continuing to do lots of lab work to come up with CAR T-cell therapies that will have improved efficacy and less toxicity,” Dr. Kochenderfer said. While maintaining that multiple myeloma “is one of the malignancies for which CAR T-cell therapy holds great promise, we still have a ways to go,” he acknowledged.
Also at the 2016 ASH annual meeting, Edward A. Stadtmauer, MD, Chief of Hematologic Malignancies at the University of Pennsylvania, commented, “The age of cellular immunotherapy for myeloma is upon us.”
But although remarkable responses have been seen with BCMA and CD19 genetically modified T-cell therapies in patients with multiple myeloma, Dr. Stadtmauer cautioned, “Still, only the minority of patients respond. We need to further engineer these products for improved activity, persistence, and decreased toxicity.”
PD-1 & PD-L1 Checkpoint Inhibitors
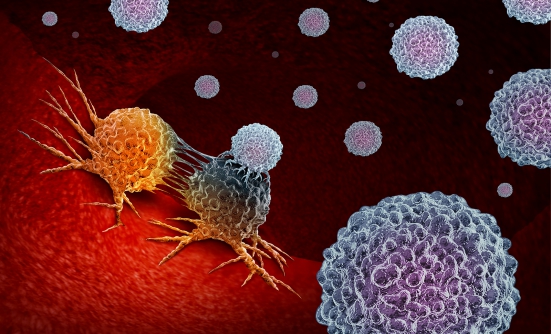
Several immunotherapy drugs known as checkpoint inhibitors have been approved by the FDA for several types of cancer, but not yet for multiple myeloma. These drugs work by blocking a pathway that protects tumor cells from the immune system’s surveillance system. This pathway includes 2 proteins called PD-1, which is expressed on the surface of immune cells, and PD-L1, which is expressed on cancer cells.
The PD-1 and PD-L1 proteins unite to form a shield for cancer cells (that is, a protection for those cells). Drugs that can stop (or inhibit) this function are able to help the immune system to find and destroy cancer cells.
The anti-PD-1 immunotherapy drugs Keytruda (pembrolizumab) and Opdivo (nivolumab), and the anti-PD-L1 immunotherapies Tecentriq (atezolizumab) and Bavencio (avelumab), have been approved by the FDA for several types of cancer, and at least 2 of them are currently being studied in clinical trials in patients with multiple myeloma, and they are beginning to show benefits in some people.
For example, in a study that combined anti-PD-1 Keytruda with immunomodulatory drugs that are already approved for the treatment of patients with multiple myeloma, including Revlimid or Pomalyst (pomalidomide) plus dexamethasone (a steroid), 75% of patients with multiple myeloma who had stopped responding to other treatments, responded to this 3-drug combination that involved an anti-PD-1 drug. In this study, in some patients the myeloma cells could no longer be seen on PET scans. This response with no evidence of disease progression lasted, on average, about 10 months.
What’s Next?
Research on immunotherapies for multiple myeloma is still in its infancy, and several of these treatments are only available in clinical trials, including 2 monoclonal antibodies and the use of combinations of currently approved drugs plus a checkpoint inhibitor.
These combinations are also being studied only in patients for whom conventional drugs have stopped working. They will need to prove safe and effective in more patients with multiple myeloma before they are approved by the FDA for general use, but researchers are hopeful that this day will come.
Currently, 2 anti-CD38 monoclonal antibodies are being investigated in clinical trials for the treatment of patients with multiple myeloma—the most advanced in development is known as SAR650984 (isatuximab), which has shown promise for relapsed multiple myeloma, and MOR-202.
“Myeloma has become a chronic illness in many patients,” suggested Kenneth C. Anderson, MD, a nationally renowned multiple myeloma expert at Dana Farber Cancer Institute in Boston, who talked at a press briefing at the 2016 ASH meeting.
“As we have more classes of novel agents, especially immunotherapies, it [multiple myeloma] will become a chronic illness with curative potential,” Dr. Anderson predicted.
Patient Resources
International Myeloma Foundation
www.myeloma.org
Multiple Myeloma Research Foundation
www.themmrf.org