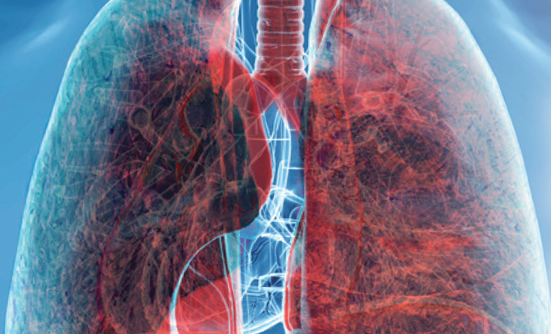
A new study found that untreated patients with advanced non–small-cell lung cancer (NSCLC) who received a combination of 2 immunotherapy drugs—nivolumab (Opdivo) and ipilimumab (Yervoy)—had increased overall survival (OS) compared with patients who received chemotherapy. In short, the patients on the immunotherapy drug combination lived longer.
In a clinical trial, measuring OS is one way of measuring the effectiveness of a new treatment.
Importantly, the benefit of nivolumab and ipilimumab was seen in all patients who participated in this study, regardless of their programmed death ligand 1 (PD-L1) expression status.
What is PD-L1?
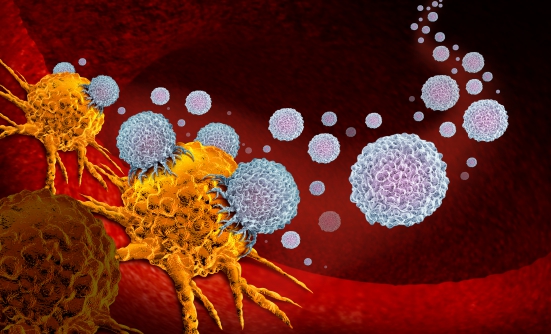
Cancer immunotherapy helps the body’s own immune system to recognize and fight cancer cells, and PD-L1 is a protein that keeps the immune system from attacking nonharmful cells in the body. However, some cancer cells have high amounts of PD-L1 and can “trick” the immune system into leaving them alone. The immune cells see these cancer cells as nonthreatening, and the cancer cells avoid being attacked as the foreign, harmful substances that they are.
One approach to fighting cancer is by blocking the PD-L1 protein. Historically, patients whose cancer cells have high amounts of PD-L1 have responded favorably to immunotherapy treatment, but patients who express low amounts of PD-L1 do not tend to do as well.
Nevertheless, researchers on this study observed an immunotherapy benefit in all patients who participated on the trial, regardless of their PD-L1 expression status. This means that this particular immunotherapy combination could help more patients, no matter how much PD-L1 they express.
According to the study’s first author, Solange Peters, MD, PhD, from the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, this dual immunotherapy approach represents a potential new first-line treatment option in advanced NSCLC and provides a chemotherapy-free treatment option for these patients.
These results come from a final analysis of part 1 of the phase 3 CheckMate-227 trial. Dr. Peters presented the results at the 2019 European Society for Medical Oncology Congress in Barcelona.
A “Practice-Changing” Drug Duo
“In my opinion, these data are practice changing,” said Dr. Peters. “We already have several front-line treatment options for [treatment-naive patients with metastatic NSCLC], including chemotherapy combined with an anti–PD-1 agent or an anti–PD-L1 agent alone. And now we have a chemotherapy-sparing option of nivolumab plus ipilimumab.”
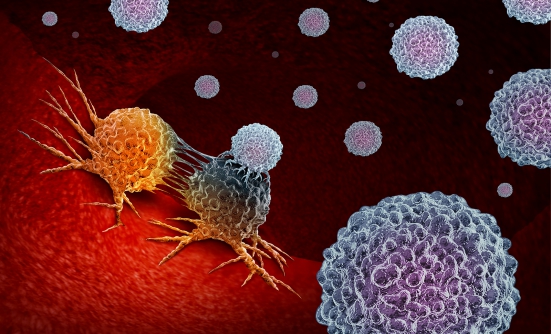
Nivolumab, a programmed death 1 (PD-1) antibody, and
ipilimumab, an anti-cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) antibody, are types of immunotherapy with different but complementary mechanisms of action.
PD-1 and CTLA-4 are both proteins found on T cells (a type of immune cell) that help keep the body’s immune responses in check. Immune checkpoint inhibitors like nivolumab and ipilimumab are used to block PD-1 and CTLA-4, and when these proteins are blocked, the “brakes” on the immune system are released and the ability of T cells to kill cancer cells is increased.
This was the first phase 3 clinical trial to show that combined PD-1 and CTLA-4 inhibition is effective in treating patients with NSCLC.
Benefit Seen Across the Board
Patients in the study had stage IV or recurrent NSCLC with good performance status and had received no prior systemic therapy. Participants also had no sensitizing EGFR mutations or known ALK alterations, and no untreated brain metastases. Nivolumab was given at a dose of 3 mg/kg every 2 weeks, and ipilimumab at a dose of 1 mg/kg every 6 weeks.
Patients were enrolled into 2 separate groups according to their PD-L1 status. In the cohort of over 1000 patients with PD-L1 expression higher than 1%, the median OS (the length of time that half of the patients in the study are still alive) with nivolumab plus ipilimumab was 17.1 months compared with 14.9 months with chemotherapy treatment. The 1- and 2-year OS rates were 63% and 40% with nivolumab plus ipilimumab and 56% and 33% with chemotherapy, respectively.
In the more than 500 patients with PD-L1–negative tumors, the benefit was still seen, with a median OS of 17.2 months with nivolumab plus ipilimumab compared with 12.2 months with chemotherapy. The 1-year OS rates with nivolumab plus ipilimumab and chemotherapy were 60% and 51%, respectively; the 2-year OS rates were 40% and 23%.
This OS benefit also translated to a benefit in overall response rates (the proportion of patients who have a partial or complete response to therapy), with 36% for nivolumab plus ipilimumab compared with 30% for chemotherapy. There was also a higher proportion of patients with complete responses in the immunotherapy arm: 5.8% versus 1.8%.
“But more importantly—and strikingly—to me was the duration of response, with a major benefit in favor of nivolumab plus ipilimumab: 23.2 months median versus 6.2 for chemotherapy,” Dr. Peters said. “This represents half of the patients at 2 years of follow-up still being in response in the immunotherapy arm.”
When the investigators looked at all patients in the study, regardless of PD-L1 status, median OS was still 17.1 months with the immunotherapy combination, compared with 13.9 months with chemotherapy.
The benefit of nivolumab plus ipilimumab was also seen across all important subgroups in the study (ie, age cohort, smoker/nonsmoker, male/female).
As for side effects, treatment with nivolumab plus ipilimumab led most commonly to diarrhea, rash, and fatigue, whereas the most common adverse events with chemotherapy were fatigue and gastrointestinal and blood toxicities. Although toxicities in the 2 arms were different in nature, they were comparable in severity.
“We used a low dose of ipilimumab to make it tolerable,” said Dr. Peters. “Doing this led to a low rate of discontinuation and treatment-related toxicities or deaths. So, it’s a highly manageable treatment.”
The investigators looked for a predictive biomarker of response but were unable to identify one after looking at various strata of PD-L1, high/low tumor mutational burden, or a combination of both. In other words, they don’t yet know which patients will respond best to this treatment.
“So, of course the next step is to try to identify a predictive biomarker of response for ipilimumab plus nivolumab versus chemotherapy,” she said.