Wouldn’t it be odd—and painful—if there were more than 200 ways to treat a broken leg? If you needed immediate attention, how could you choose the best treatment? Would you have the endurance to try 2, 3, or 4 therapies to fix your broken bone?
Fortunately, there are prescribed ways to deal with most diseases and injuries of the body. Physicians don’t bat an eyelash over a broken leg—they reset the bone, put the leg in a cast, and wait 6 to 8 weeks. Cancer treatments aren’t always as clear-cut as handling broken bones, but they operate similarly.
Maintaining the Mind
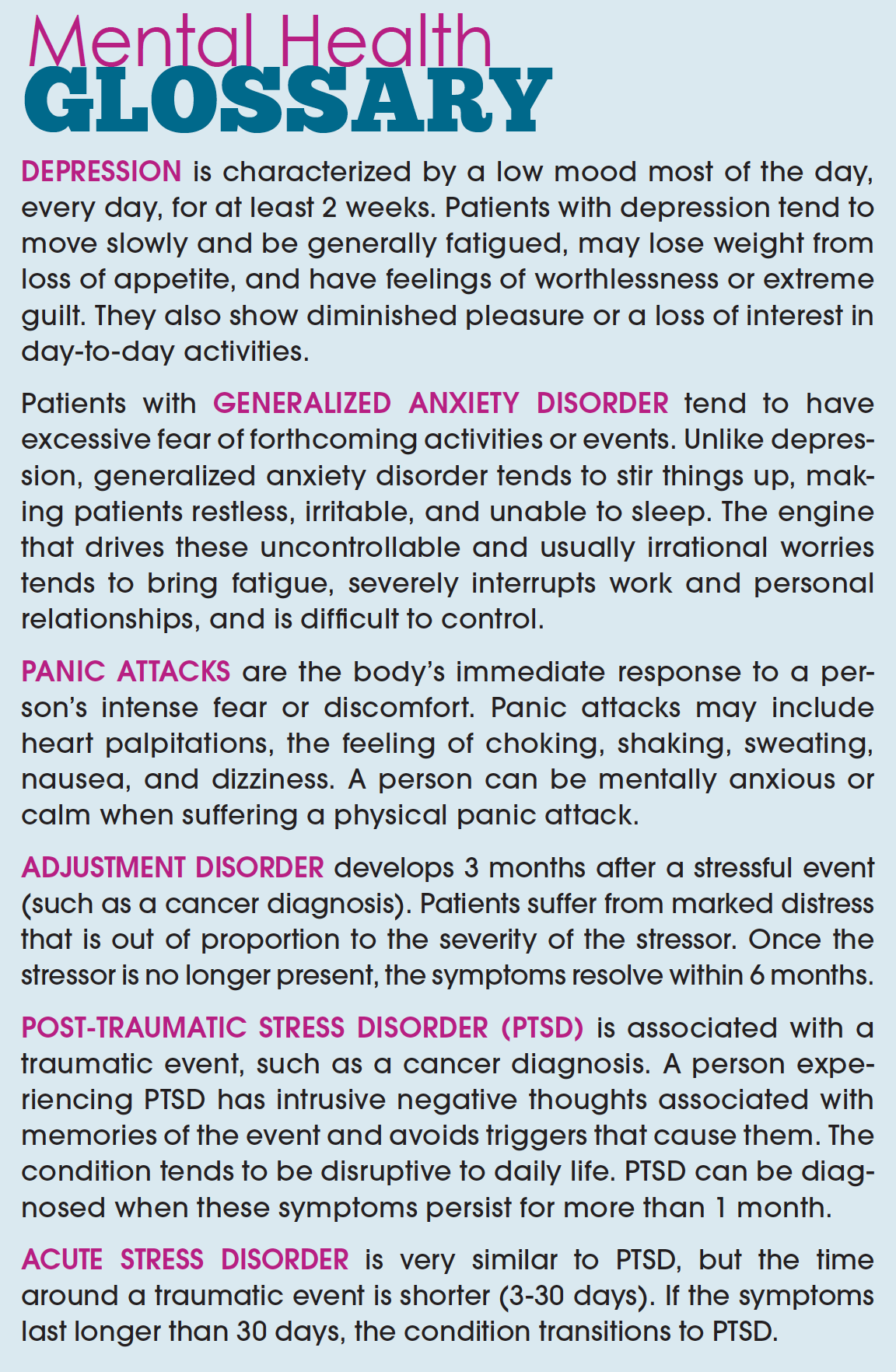
Although somatic treatments operate mostly according to rule, the arena of mental health diagnoses and treatments can feel like the lawless terrain of the Old West. Are you on edge because you’re worried about chemo’s side effects, or do you have a generalized anxiety disorder? Are those just unpleasant memories, because you go into the hospital for your 3-month checkup, or are you suffering from post-traumatic stress disorder (PTSD)?
Patients don’t often march through survivorship without some experience of mental health challenges. “Cancer is a distressful situation, which is normal. Pervasive or persistent mental health symptoms may indicate that you need professional help,” says Amelia Baffa, Advanced Clinical Nurse, Angie Fowler Adolescent & Young Adult (AYA) Cancer Institute, University Hospitals of Cleveland. “If you had physical pain, you’d find a doctor. Mental health, on the other hand, is often stigmatized,” she adds.
Instead of a cakewalk toward therapeutic options offered in survivorship, patients often have to 2-step their way to mental clarity. The first step is rooted in observation of the symptoms, their intensity, and the kind of impact they have on a person’s day-to-day experience. For example, is the patient occasionally tired, or is he or she unable to get out of bed? Being tired all the time may be a symptom of depression.
The Difficulties of Mental Health Diagnosis
The issues Ms. Baffa observes most often in AYAs include the full mental health spectrum, such as major depressive disorder (depression), generalized anxiety disorder, panic attacks, adjustment disorder, acute stress disorder, and PTSD. Their symptoms and intensity are as diverse as the people affected by them.
“We look at basic things to gauge how the affected patients are doing. Are they sleeping? Are they eating? If they’re momentarily sad, for the day, it’s not so much a concern, but if it’s every day, all day, most days, they should seek professional help,” says Ms. Baffa.
The key points patients must determine are (1) how much, and how significant, these symptoms are in interrupting their social, academic, and occupational interactions; and (2) making sure that the symptoms are not related to another health condition, substance use, or another physical or mental health disorder.
Tackling Therapy
Once a patient has a handle on the problem, the next step is finding the right therapy. This is where the process can become overwhelming, because there are indeed more than 200 types of therapies available. Not all those therapies can be applied to every condition, and not every therapy is evidence- based. Determining the right fit depends on what a patient connects to—how the patient feels about it; whether it makes sense to the patient, and what other support the patient is getting.
To complicate matters, a therapy that works for one person may not work for another. If, for instance, a patient prefers talk therapy, would a psychiatrist or a licensed professional certified counselor be best? After that choice, the patient must establish rapport with the clinician, which may not happen with the first or second therapist. Patients new to this “mental health dance” can feel as if they’re shuffling around with 3 left feet.
If you’re looking for a cheat code to navigate the multitude of therapies available, Dr. Jennifer Giesel, PhD, LICDC-CS, Clinical Psychologist at University Hospitals of Cleveland, uses 2 basic evidence-based approaches that can help patients begin on the right foot.
The first is cognitive behavioral therapy (CBT), which is based on the idea that our thoughts—rather than external things like people, situations, and events—produce our feelings and behaviors. CBT refers to different therapies that produce effective results for a wide range of disorders, including anxiety, depression, and PTSD.
“CBT helps people catch their automatic, negative thoughts, and it challenges them to find new ways of thinking even when we can’t change the situation,” says Dr. Giesel. For instance, a cancer survivor may have severe anxiety about every required follow-up scan. CBT offers techniques patients can use to alter their thoughts to reduce the worry about it.
Thought log. One type of CBT uses a thought log. “They offer a concrete, step-by-step approach that helps patients break down their thought patterns,” comments Dr. Giesel (see Patient Resources Box).
Diaphragmatic breathing. Another tool Dr. Giesel suggests using is diaphragmatic breathing, which helps patients make physiologic changes when emotions run high. Once patients cool down, they can more easily manage the reflective work of CBT, like a thought log.
“Shallow breathing promotes fight or flight; diaphragmatic breathing reverses the physical feeling of panic or anxiety, which, in turn, decreases the intensity of those high emotions, and enables a patient to focus,” says Dr. Giesel.
Narrative therapy. Patients able to use thought logs and diaphragmatic breathing can add a third arrow to the quiver: narrative therapy—reconsideration of the stories of their cancer encounter. This technique finds and treats pieces of the stories that hamper growth and understanding. As part of my work with male cancer patients and survivors, I encourage patients and survivors to reframe their cancer narratives to become heroes in their own stories, rather than victims.
Everyone going through cancer encounters falls and challenges. The key is to find the opportunities that have come from these challenges, not just to tack each one up on a wall in your mind as one more tough experience. When patients are stuck to an unprocessed, particularly traumatic experience, I believe a person’s life is held back, and their quality of life suffers.
People’s views—their personal beliefs, expectations, and philosophies—form meaning from cancer, and the ways they go about telling their cancer story. Many variables govern the narrative, when the story starts and stops, exaggerated or diminished parts, as well as the voices of others who are included or excluded in the story. Pull the levers on one or more of those variables, and out plops a new version.
When a cancer diagnosis hits, a patient’s task is single and clear: how to stay alive. In survivorship, with its associated opportunities and built-in challenges, choices multiply and become less clear. The path to finding and enjoying the right opportunities is through evidence-based therapies, tapping into a support system, and as Ms. Baffa advises, “don’t isolate yourself—you don’t have to suffer in silence.”
This article is based on a presentation at CancerCon 2017 by the author; Amelia Baffa, Advanced Clinical Nurse, Angie Fowler Adolescent & Young Adult Cancer Institute, University Hospitals, Cleveland, Ohio; and Jennifer Giesel, PhD, LICDC-CS, Clinical Psychologist, University Hospitals, Cleveland, Ohio.
Patient Resources
M Powerment
www.m-powerment.org/wpcontent/uploads/2017/04/CancerCon-presentation.pdf
Thought Log
www.m-powerment.org/wpcontent/uploads/2017/04/ThoughtRecord.pdf
Narrative Reframing Exercise
www.m-powerment.org/wpcontent/uploads/2017/04/Narrative-Reframing-Worksheet.pdf