Chimeric antigen receptor (CAR) T-cell therapies, already indicated for the treatment of refractory non-Hodgkin lymphoma and relapsed/refractory acute lymphoblastic leukemia (ALL), may soon become a standard treatment alone or in combination with immune-modifying agents in chronic lymphocytic leukemia (CLL).
Although the treatment appears promising, a suboptimal number of patients with advanced CLL have shown a durable response to CAR T-cell therapy, and investigators are looking at ways to enhance durability.
CAR T-cell therapy is a form of immunotherapy in which a patient’s T-cells are removed from the blood and expanded in the laboratory, after which the gene for a CAR is added to the T-cells. The manufactured T-cells are then reinfused into the patient. The added CAR binds to an antigen on the patient’s tumor cells, allowing them to kill the tumor. It is considered a “living drug,” with effects that are durable and persistent after infusion.
Identifying patient characteristics that predict responses to therapy will be critical to the emergence of CAR T-cells for use in CLL. The CAR T-cell treatment holds the potential for use in patients with relapsed or refractory CLL, and possibly in earlier lines of therapy, as well.
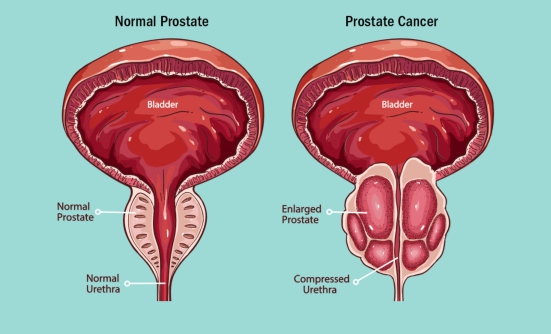
A form of CAR T-cell therapy directed against patients with heavily pretreated CD19-positive hematologic cancers demonstrated the feasibility of CAR T-cell therapy in patients with CLL. In that study, 2 patients with CLL who were resistant to chemotherapy showed sustained remission with follow-up of at least 8 years, after CAR T-cell therapy.
In another study of CD19-targeted CAR T-cell therapy, at a median follow-up of 19 months, 8 of 14 patients with advanced CLL (57%) had a response to therapy, including 4 complete responses. Other studies using this same type of CAR T-cell treatment in CLL have demonstrated response rates from 12% to 100%. These response rates are generally lower than those seen in ALL.
Predicting the patients who will have a response is one obstacle to CAR T-cell therapy in CLL. It is possible that defects in T-cells in patients with CLL may prohibit expansion of the CAR T-cells, reducing the chance of response.
Using oral kinase inhibitors, such as acalabrutinib and ibrutinib, may have an immune-stimulating effect by improving the function of those T-cells, which could enhance the activity of CAR T-cells in CLL. Combinations of kinase inhibitors and CAR T-cell therapies are underway.
For example, the combination of ibrutinib and CAR T-cell therapy was tested in 19 patients with CLL who did not achieve a complete remission despite having been treated with ibrutinib for at least 6 months. In this study, with a median follow-up of 18.5 months, 18 of the 19 patients (95%) remained alive. Some 94% of the patients had no disease in their bone marrow.
Eventually, CAR T-cell therapy may be used in CLL for earlier lines of treatment (over biologic therapies) because of the short treatment duration and high rates of what is known as minimal residual disease (MRD). MRD is a term to describe a small number of cancer cells in the body after cancer treatment, and correlates with a longer survival without disease progression. CAR T-cell therapy may also be a better option in patients not likely to respond to other therapies, such as patients with resistance to kinase inhibitors.