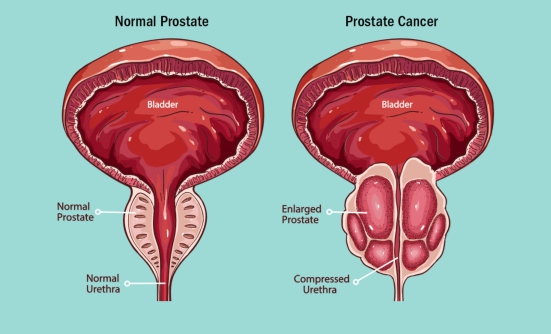
Immunotherapy has led to great advances in the treatment of patients with advanced bladder or kidney cancer, but determining whether such therapy is curative is still unclear, said Thomas Powles, MD, PhD, FCRP, Director of Barts Cancer Centre, and Professor of Urology Cancer, Barts Cancer Institute, London, England, at the 2021 ASCO Annual Meeting.
According to Dr. Powles, getting closer to cure with immunotherapy depends on advances in 3 areas— discovery of more biomarkers that drive the development of cancer; the use of combinations of 2 immunotherapies, which has made a significant difference in kidney cancer, but in bladder cancer, antibody-drug conjugates are now showing more promise; and the development of new immunotherapies.
Complete Radiologic Response
Dr. Powles asked if a complete response to therapy, as demonstrated by radiologic images that don’t show any sign of cancer (and is therefore called “complete radiologic response”), can mean cure of the cancer.
“In advanced disease, complete radiologic response probably correlates with cure, but certainly, it’s not an accurate assessment of cure,” Dr. Powles said.
The reason for this is that the complete radiologic response rates seen with different first-line immunotherapies in patients with advanced blad- der cancer (and kidney cancer) are all fairly similar. Therefore, according to Dr. Powles, looking at these data is not the best way of picking the “winners,” or the best treatments.
He described a study in which the average time without disease progression (also called “disease-free survival”) for patients with bladder cancer who received maintenance treatment with the immunotherapy Bavencio (avelumab), a PD-1 inhibitor, after they had a complete response to chemotherapy was measured in months, not in years, meaning that the average response to the immunotherapy was less than 1 year.
“You would expect complete response with chemotherapy to be associated with a disease-free survival measured in years if it was cure,” he said.
When using the immunotherapy combination of Opdivo (nivolumab), a PD-1 inhibitor, and Yervoy (ipilimumab), a CTLA-4 inhibitor, about one-third (33%) of patients with intermediate- and poor-risk advanced kidney cancer achieve an ongoing response, and similar rates are seen with maintenance immunotherapy with avelumab in bladder cancer.
“This is really quite impressive,” he said. “But remember these patients continue on therapy; some of them may be cured, and indeed, there are data from kidney cancer suggesting you may be able to stop therapy in some patients. This is controversial, but nevertheless, we are beginning to get there.”
How Can We Cure More Patients?
According to Dr. Powles, selecting the appropriate patients who may be candidates for specific treatments is extremely important, especially when designing clinical trials. Targeting certain cancer biomarkers—proteins, molecules, and other genetic markers that affect how cancer cells behave—is a common method used to tailor treatment to each patient. However, in using these biomarkers to target treatment, especially treatment based on the PD-1 or PD-L1 expression on cancer cells, researchers don’t always hit the nail on the head.
Dr. Powles says that oncologists should “step away” from using the PD-1/PD-L1 biomarker in bladder cancer (and also in kidney cancer) and instead use VEGF-targeted drugs in combination with immunotherapy.
However, in terms of determining patients’ response to immunotherapy, classifying patients according to their molecular (or biomarker) subgroups— and targeting treatment based on specific biologic markers and immune characteristics—has proved more promising in kidney cancer.
In bladder cancer, tracking the circulating tumor DNA biomarker for FGFR alterations in the blood has also demonstrated some success in predicting response to targeted therapy against the FGFR mutation. In addition, the alterations found in circulat- ing tumor DNA are similar to what is found by taking tissue samples. “So we may be able to move away from tissue-based biomarkers in the future,” he said. “That would be exciting.”
Promising Drug Combinations
Curing more people with advanced bladder or kidney cancer will also involve improving the drugs available to patients, according to Dr. Powles.
To get better results, doctors should start by using 3-drug combinations, such as Cabometyx (cabozantinib), ipilimumab, and nivolumab in bladder cancer, instead of the 2-drug combinations that are now used in bladder and in kidney cancer. Clinical trials have shown that patients have higher response rates to 3-drug combinations than to 2-drug combinations.
“But will we cure more patients? I don’t know the answer to that yet,” Dr. Powles said. “Certainly, in testicular cancer, for example, you need to give the drugs together to maximize outcome.”
Many drugs are showing promise when used in combination with other immunotherapies, especially the combination of a CTLA-4 inhibitor plus the new antibody-drug conjugates in bladder cancer.
Novel and exciting approaches also include looking at new immunotherapy drugs, as has been done in lung cancer with the investigational immunotherapy tiragolumab in combination with the PD-L1 inhibitor Tecentriq (atezolizumab).
“We should be doing these experiments in bladder cancer,” Dr. Powles said.
Finally, introducing these drugs in early-stage disease is of critical importance. Research in bladder cancer has shown that immunotherapy combinations and immunotherapy plus chemotherapy combinations don’t seem to be better than using 1 immunotherapy alone. “This is something we’re going to need to think carefully about,” he said.