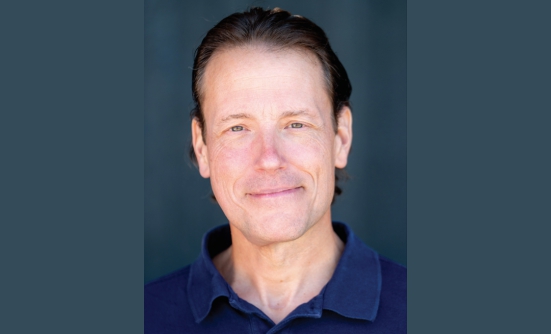
In October 2014, I was feeling unusually run down, and I assumed I had the flu. I was training for several long races in 2015, so the fatigue, aches, and pains weren’t alarming. They were my badge of honor, but when this all affected my ability to move, I finally went to my primary care physician, who did a blood test. He called a day later to let me know that I did not have the flu, but I was anemic, which was unusual for someone like me. I was only 43, I ran about 20 to 30 miles a week, and was careful about what I ate. He told me to come back for another blood test.

I forgot all about it for a month, although the fatigue didn’t dissipate, and I was having intermittent migraine headaches, which I had never had before. The doctor called to say they found “something” in the blood test, and I should see some specialists. On December 24, 2014, Dr. Thrash called to say that he had made an appointment for me with an oncologist.
The idea that I might have cancer had never crossed my mind before I pulled into the parking lot of Asheville Oncology. Until then, I was just following my doctor’s orders. Cancer happens to other, less healthy, people. I was as likely to have cancer as I was to grow an extra toe.
Learning Fast
Dr. Vashist, the oncologist, said that I had proteins that were replicating themselves too fast. I knew what he meant. Cancer. Until that moment, I hadn’t heard of multiple myeloma, but after several depressing late nights stalking Google and every website I could find on the subject, I learned it was a blood cancer that often creates lytic lesions (essentially, holes) in bones, frequent infections, reduced kidney function, and low red blood cell count, and that more than 30,000 new cases were diagnosed each year in the United States. I didn’t have any common risk factors, such as obesity or older age.
The first step, Dr. Vashist said, was to get a second opinion, to determine the next course of treatment. Multiple myeloma is a complicated blood cancer, and many new treatments are becoming available.
I visited 2 other multiple myeloma specialists before choosing Winship Cancer Center at Emory University Hospital in North Carolina. Myeloma expert, Sagar Lonial, MD, and his team, investigated some options before deciding on a treatment plan.
After a second bone marrow biopsy and a PET scan, the team discovered that 80% of my plasma (blood) cells were cancerous, and I had lytic lesions in my bones, including my skull, hip, sternum, ribs, and spinal cord. Two compression fractures had already begun to heal themselves.
Coping without Running?
The lesion in my left hip was the most concerning, so they told me that I had to stop running—immediately. I felt betrayed. It was a gut punch not to be able to run. This led me to despair for several days. Running had become my identity and my coping mechanism. I processed the tough days through running, and celebrated great days with movement. How was I supposed to process one of the most difficult times of my life without running, especially if my life was about to get a lot shorter?
I have a wife and 3 kids. At the time, the children were 14, 11, and 18 months. Would I see any of them grow up? I was morbid, but this was understandable: there were many unknowns.
Coping was hard, but I found the swimming pool. I started swimming laps, something I hadn’t done since I was a high school senior. It was hard at first, but after watching others who seemed to know what they were doing, and trying to not be so self-conscious, I found my stride in the water.

Myeloma Therapy
My treatment began with the “holy trinity” of drug combinations for multiple myeloma with dexamethasone, Revlimid, and Velcade, before a bone marrow transplant. To assist my bones’ repair process, I received regular infusions of Zometa. The cancer responded well to the drugs, but I didn’t achieve complete remission until I had a bone marrow transplant in August 2015.
I was in the hospital, out, in again, and then near the hospital for nearly 5 weeks before the heart catheter was removed, and I was allowed to return to Asheville. During my hospital stay I moved as much and as often as I was permitted or able, despite being discouraged from “overdoing it.” When I came home, I didn’t have any hair, and not much energy, but I wanted to feel better, so I kept moving.
Keep Moving
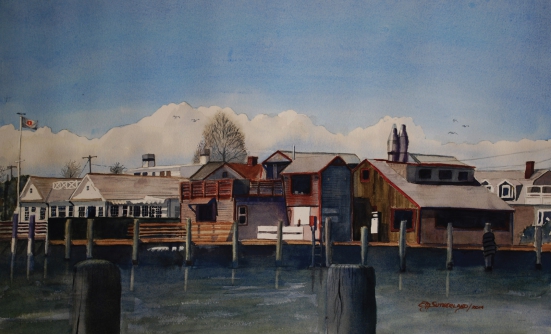
I wanted to keep running, or at the very least, moving. Living a healthy and active lifestyle before my diagnosis helped me recover quickly, and I wanted this to also be a part of my life after treatment. Because my immune system was still compromised, I had to be careful with interactions at high-risk places, such as malls and gyms. I am fortunate to live by a lake with a half-mile walking trail, where I spent as much time as I could. By the end of November 2015, I was given the green light to begin light jogging.
Calling this “jogging” is very generous, but I was moving, and increasing mileage every week. By the end of January 2016, I ran my first 10K race. It was slow, painful, and not much fun. I cried when I crossed the finish line.
By the end of 2016, I completed 16 races, including 3 half- marathons and an intense 18-mile trail race with 5,000 feet of elevation. I wanted to use this opportunity to fill in the gaps that we felt as a family. My disease wasn’t in remission, and I continued with maintenance chemotherapy and doctor’s appointments after the transplant. Staying alive, more than ever, meant being persistent, and adjusting to a new normal. It’s not easy, and next to impossible to do on your own.
The Different Obstacles of Cancer
Objectively, cancer is hard. It’s scary. There are many unknowns, and until there is a cure, we have to live as long and as well as we can with all sorts of obstacles. It’s even harder when you have difficulty being active, because you are in pain or very tired, or you struggle to pay the electric bill because you haven’t been able to work as before, if at all.
Maintaining a healthy and active lifestyle is tough enough even when you don’t have cancer. When your bones start to ache and you’re scared you might injure yourself, it’s easy to give up. Aside from my age, which was young compared with many patients with multiple myeloma who are usually in their 60s, one major advantage I had during treatment was that for many years before diagnosis, I had made movement and running a part of my lifestyle.
Other than having cancer, I was very healthy, active, and ate healthy food. Thanks to my activity level before, during, and after treatment, my care team was able to use the most aggressive treatments to combat the disease. Although I was not diagnosed early, my self-medicating activities were, and still are, paying off.
Financially, we nearly lost everything. If it weren’t for fantastic friends and family, I don’t know how we would have overcome the loss of my income. Because of the amount of time spent at doctor’s offices, infusions, or recovering from treatment, we had to let my business go. Two weeks before my scheduled bone marrow transplant, friends held a music benefit for us at a local venue, just so that we could pay our bills for a couple of weeks.
I know about struggling to pay bills, and how scary it can be to think that you’re letting everyone down—and there’s not a damn thing you can do about it.
Throwing Bones for Cure
At the beginning of 2017, I formed Throwing Bones, a nonprofit organization. The name alludes to the effect that multiple myeloma has on our bones, pays homage to my love of jam bands (such as the Grateful Dead), and refers to rolling dice or reading the future. The future is like a crapshoot, but we’re going all in. We’re going to throw those bones and let them ride.
Through Throwing Bones, we are planning several races each year, to benefit our Keep Moving Forward program to encourage patients to stay healthy and active during and after treatment, and our Patient Assistance Fund, to assist patients with multiple myeloma and their caregivers who are facing non-medical financial hardships.
We are still in debt despite having insurance. In addition to seeing my local oncologist, which requires regular travel, I travel to Atlanta every 4 to 6 months, which is more than 4 hours away. The multiple myeloma patient community needs a lot of help with hidden costs, such as travel to and from treatment. Through our Patient Assistance Fund, patients can apply for grants for financial assistance to help pay for treatment, medical bills, travel to medical facilities, or even household expenses.
From April 1, 2018, to May 24, 2018, I ran 1,175 miles on the Mountains to Sea Trail from the Outer Banks of North Carolina to Clingmans Dome on the Appalachian Trail at the border of North Carolina and Tennessee. We raised nearly $70,000 for Throwing Bones’ mission.
In 2019, we hope to establish a pilot clinic to assess patients’ physical ability. We are planning 3 running events—including our second year of Throwing Bones Trail 5K/10K—to raise awareness of Throwing Bones, and we hope to give grants to patients and caregivers.
Throwing Bones isn’t going to cure multiple myeloma, but I hope we can encourage and inspire every patient until an inevitable cure happens.
Patient Resources
Throwing Bones
www.throwing-bones.org
Multiple Myeloma Research Foundation
https://themmrf.org/