Genetic counseling and testing may be recommended right after a cancer diagnosis or years after you have been told you are cancer-free. The referral may be because of the specifics of your cancer diagnosis, or it may be related to your family history of cancer. Regardless, many patients enter genetic counseling with no idea what to expect.
Cancer genetic counselors work with individual patients, families, and physicians to determine if a cancer or a family history of cancer has a hereditary cause. A genetic counselor will guide you through the cancer genetic testing process, providing explanation and support at each step.
Why Genetic Counseling?
Genetic counseling can be provided in several ways. Traditionally, you would meet in person with a genetic counselor. With the growing demand for these services, newer methods, such as a video or telephone chat, have become common. Regardless of how you connect with your genetic counselor, the topics covered will likely be similar.
First, you will be asked about your medical history and many generations of your family cancer history. The family history typically includes cancer history questions about parents, siblings, children, aunts, uncles, grandparents, and cousins. It is useful to come prepared with information about cancer diagnoses in the family, including cancer type and age at diagnosis. For family members who did not have cancer, the genetic counselor will want to know how old they are, or were at death.
You may know what cancer your great grandmother had, or you may know very little about the cancer history of your family. Either way, you should provide as much information as you know. The genetic counselor will use this information to detect any patterns of hereditary cancer, identifying which conditions (if any) should be ruled out, and what testing to offer.
Inherited Cancer Conditions
Often, the genetic counselor will review some information about cancer genetics and the specific hereditary cancer conditions for which your personal or family history is suspicious. The genes discussed can range from relatively common and well-known genes, such as the BRCA genes (associated with breast and ovarian cancer), to much rarer conditions, such as the SDH genes (associated with paragangliomas). The information covered will be specific to you and your family history.
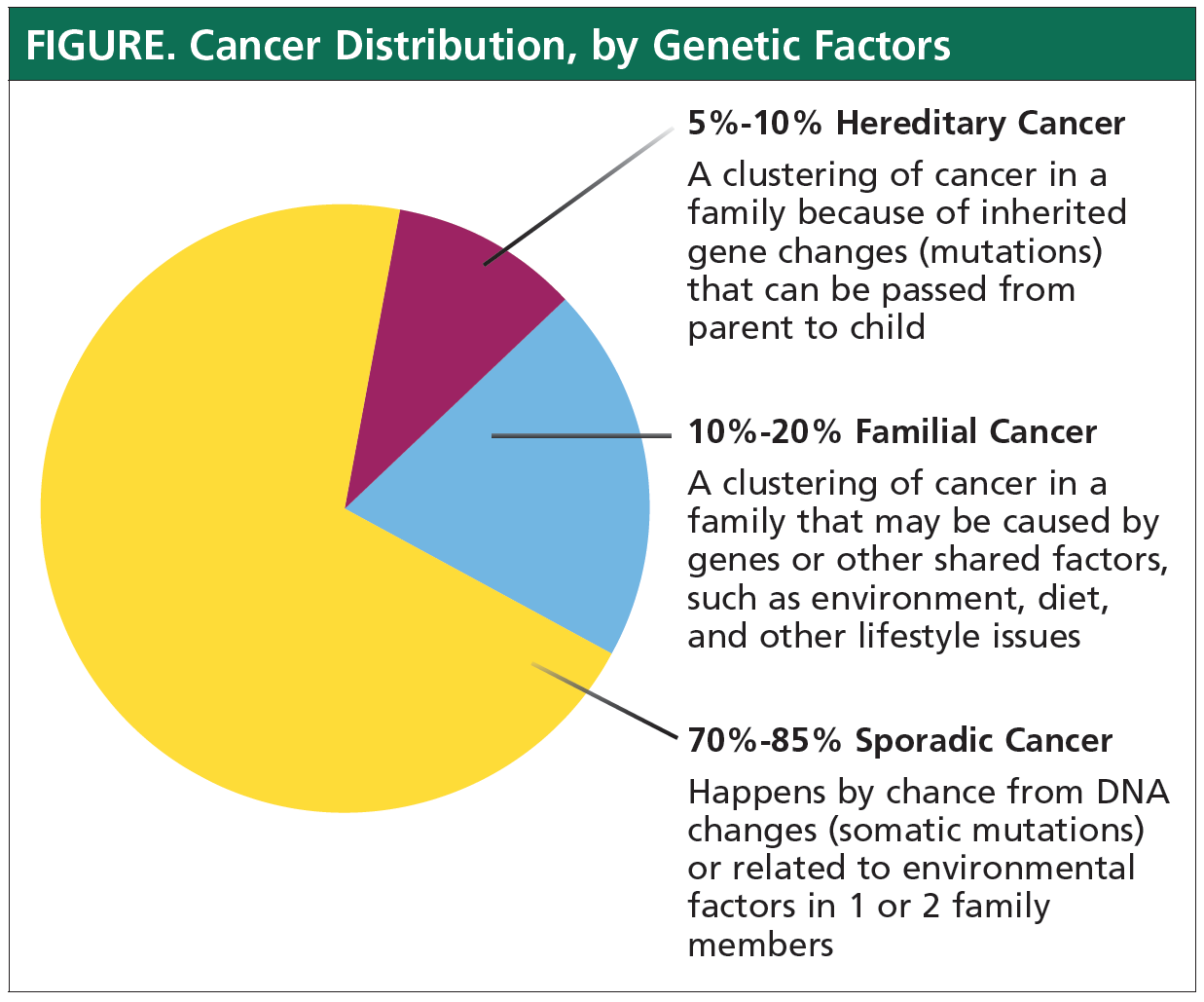
When no hereditary cancer condition has been diagnosed in the family, remember that only 5% to 10% of all cancers are caused by an inherited cancer condition (see Figure). Genetic counselors provide information about specific conditions to illustrate how cancer risks are increased and how treatment changes when one of these conditions is found. In most cases, you will not have the specific condition discussed in your counseling session.
Genetic Testing for Hereditary Cancer
Often, you may be recommended to have genetic testing for a group of hereditary cancers. This is called “panel genetic testing” and has become increasingly common in cancer genetics. Many hereditary cancer conditions share the same types of cancer and are very difficult to identify based on the family history alone. For example, more than 10 genes are known to be associated with an increased risk for breast cancer. The panel genetic testing for colon cancer can include up to 20 genes.
Your genetic counselor should review your testing options, including panel testing. With a full understanding of the pros and cons of different options, you will be able to decide which test is right for you.
Understanding Test Results
In addition, a genetic counselor will review the possible genetic test results. The language of genetic test results can be tricky. A “positive result” means that a mutation (a harmful change in a cancer gene) has been identified, and you have a hereditary cancer condition. A “negative result” means that no mutations were found in any of the tested genes. But test results can come back as uncertain or inconclusive. This means that a genetic change was found, but it is not known whether that change is harmful or harmless.
Most uncertain test results are found to be harmless once scientists learn more about the specific mutation. However, it can take months or years for this information to be discovered. In the meantime, uncertain results are treated the same as negative results.
Positive test results. If your test is positive, your genetic counselor will review the cancer risks and treatment recommendations for your specific condition. Together, you and your medical team will determine the best treatment plan for the cancer and for prevention of cancer in the future. Family members who are also at risk for having the gene mutation will be identified. Genetic counselors help in informing your relatives of your test results and directing your relatives to a local genetic counselor for testing.
Learning that you have a hereditary cancer condition is an emotional and medical experience. Genetic counselors provide support, answer your questions, and advocate for your care with your medical team.
Negative test results. If your test is negative or inconclusive, your genetic counselor may still provide recommendations based on your personal and family history. Approximately 20% to 30% of all cancer is familial (to differentiate from inherited cancer), meaning there is no known mutation in the family, but cancer is clustering in the family. This is likely a result of a combination of multiple genes with smaller effects on cancer risks and environmental factors.
For example, a family may have a family diet high in red and processed meat, a high incidence of inflammatory bowel disease (IBD), and multiple family members with colon cancer. This diet and IBD are risk factors for colon cancer. If genetic testing is negative, this family has familial clustering of colon cancer from environmental (diet) and genetic (predisposition to IBD) factors. Another example is a family with fair skin, a history of repeated sunburns, and multiple family members diagnosed with melanoma. Fair skin and sunburns are risk factors for melanoma. If the genetic testing is negative, this family has familial clustering of melanoma from environmental (sunburns) and genetic (fair skin) factors.
Because of familial clustering, relatives of a person with cancer may be recommended to have cancer screening more frequently, or at an earlier age, than other people. The children of a man diagnosed with colon cancer at age 46 should begin colon cancer screening with a first colonoscopy at age 36, even if no genetic mutation was identified on their genetic testing.1
Does Your Insurance Cover Genetic Testing?
A genetic counselor may also review some practical issues related to genetic testing, including health insurance coverage. Insurance coverage for cancer genetic testing is often based on specific criteria set out by different insurance companies. These criteria include patterns associated with hereditary cancer conditions, such as cancers at an early age, multiple cancers in the same person, or the same or related cancers in several family members. If these criteria are met, Medicare and private insurers typically offer good coverage for testing. Your genetic counselor will assess whether you meet your insurance’s criteria.
Depending on your coverage and deductible, even if your insurance covers genetic testing, you may still owe part of the cost of testing. Most labs will inform you if you will have a large (more than $100) out-of-pocket cost before beginning the testing. There are also financial support programs at most major labs to help reduce the costs for qualified patients. Ask your genetic counselor what the specific billing policies are at the lab that will be used for your testing.
Patients who do not meet the insurance criteria or have high-deductible insurance plans may choose to pay for cancer genetic testing entirely out of pocket.
In the past, genetic testing cost thousands of dollars. Now, high-quality comprehensive cancer genetic testing is available at many laboratories for less than $400.
Getting the Test Results
Before leaving your genetic counseling appointment, you should have all your questions answered and a plan for next steps. If you decide to have cancer genetic testing, you should know how and when to expect your test results. Some genetic counselors provide the results in a separate appointment, and others provide the information by telephone. You may also receive a copy of your results for your records. Because every clinic handles test results differently, be sure to ask your genetic counselor what to expect.
Evolving Changes in Genetic Testing
What if you already had genetic testing? You may still wish to consult with a genetic counselor. Hereditary cancer genetic testing has advanced quickly over the past decade. New genes might have been discovered since you had your test a few years ago. Also, testing techniques have changed and can now pick up mutations in already tested genes that were not identified even 2 to 3 years ago.
Even if no further testing is recommended, genetic counselors can provide you and your family with updated recommendations based on your family history alone. Genetic counseling and testing can play a vital role in your cancer care. Because of the complexity of the test results and the emotions involved, genetic counselors can guide you through this process. With a better idea of what to expect, you will come to your genetic counseling appointment better prepared, and without anxiety.
To find a genetic counselor near you, speak with your physicians or visit www.nsgc.org/page/find-a-genetic-counselor.
Key Points
- With the growing demand for genetic counselors, newer methods, such as a video or telephone chat, have become common
- It is useful to come prepared with information about cancer diagnoses in the family, including cancer type and age at diagnosis
- The genetic counselor will use this information to detect patterns of hereditary or familial cancer and determine what testing to offer
- Insurance coverage for cancer genetic testing is often based on specific criteria set out by your insurance company; your counselor will tell you if you meet those criteria
Reference
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Colorectal Cancer Screening. Version 1. 2018. March 26, 2018. www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf.
Patient Resources
American Cancer Society
www.cancer.org/cancer/cancer-causes/genetics/should-i-get-genetic-testing-for-cancer-risk.html
National Cancer Institute
www.cancer.gov/about-cancer/causes-prevention/genetics/genetic-testing-fact-sheet
National Society of Genetic Counselors
www.nsgc.org/page/whoaregcs