This article is supported by funding from Janssen Oncology.
Expert Commentaries by Peg Rummel, RN, MHA, OCN, NE-BC, HON-ONN-CG
Since 1990, the 5-year survival rate for patients with multiple myeloma has doubled, largely as a result of treatment with combinations of newer, targeted therapies.1,2 For many patients with multiple myeloma, these groundbreaking treatments lead to years of survival with a good quality of life.3,4 To achieve these kinds of outcomes, however, patients first undergo a series of medical tests to determine what kind of multiple myeloma they have, and how aggressive it is.5,6
This testing, and the large amount of information it provides, can make the first 90 days after a multiple myeloma diagnosis a challenging time. Patients may also be working through difficult emotions and possibly dealing with some basic challenges, such as getting back and forth from doctor appointments.7 In addition, many patients with multiple myeloma are older, so they are often managing other health issues.8 But patients are not alone. With the help of healthcare providers, caregivers, and support services, obstacles can be overcome, and appropriate medications can be given, allowing many patients to achieve the kinds of promising survival results seen in clinical trials, while maintaining an excellent quality of life.
This article provides an overview of multiple myeloma, with a focus on the first 90 days after diagnosis. Each section is followed by expert commentary from oncology nurse navigator Peg Rummel, RN, MHA, OCN, NE-BC, HON-ONN-CG, who speaks from 25 years of experience.
Ms. Rummel: When I first started in the field, there weren’t a lot of treatments for patients with multiple myeloma. Now, patients have a lot more options, and over the past 2 years, the landscape has just blossomed with FDA approvals. With these new treatments, patients are living much longer.
Multiple Myeloma and Related Diseases
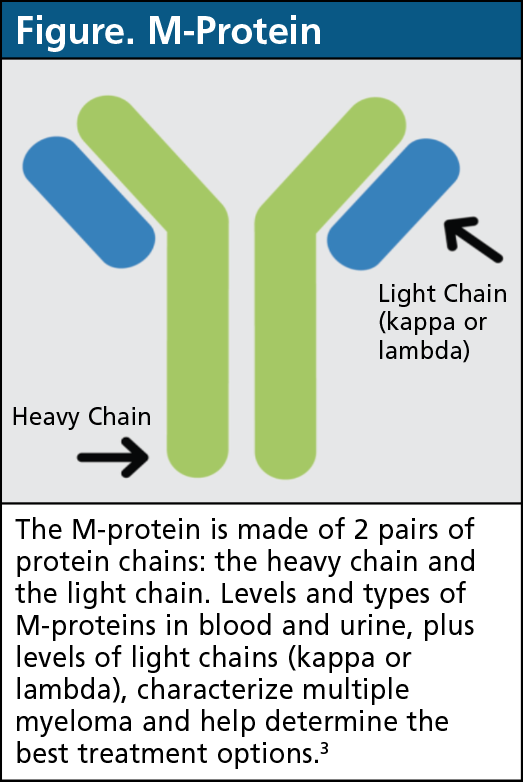
Multiple myeloma is a type of cancer that affects plasma cells, which are a type of white blood cell in the bone marrow.9 In healthy people, plasma cells make antibodies for the immune system, but in patients with multiple myeloma, plasma cells overproduce M-protein, an abnormal antibody (Figure).3 A high level of M-protein in the body can lead to a variety of symptoms involving the blood, bones, and kidneys.1
Before patients have “active” or “full-blown” multiple myeloma, they go through 2 stages of disease that are usually symptom-free: monoclonal gammopathy of unknown significance (MGUS) and smoldering multiple myeloma.10,11 MGUS, smoldering myeloma, and multiple myeloma are diagnosed by the amount of M-protein (or parts of M-protein) in the blood and urine, the number of plasma cells in the bone marrow, presence or absence of bone lesions, and symptoms.12
Ms. Rummel: With multiple myeloma, there are so many stages. There’s MGUS, there’s smoldering multiple myeloma, there’s full-blown myeloma, and each stage has its own treatment that’s constantly changing. There are many clinical trials being conducted for patients in all stages of multiple myeloma that show which treatments are appropriate for patients in each stage of their disease.
Common Diagnostics
To determine treatment options, patients need to undergo a wide range of medical tests.2,5 Common diagnostics are summarized below.
Complete blood count (CBC). A CBC measures different types of blood cells. Multiple myeloma can affect red blood cells, white blood cells, and platelets.5
Chemistry panel. This test measures other parts of blood, such as beta-2 microglobulin, a type of protein made by myeloma cells.3,5
24-hour urine protein. Higher protein levels in urine suggest more aggressive multiple myeloma. Different urine tests measure different types of proteins.3
Serum quantitative immunoglobulin testing. This measures antibodies in blood, including M-protein (Figure).3
Free light chain analysis. M-proteins are made up of heavy protein chains and light protein chains (Figure).3 This test measures the 2 types of light chains (kappa and lambda) in blood.3 The balance between light chain types can reveal disease severity.12,13
Bone survey/computed tomography (CT). All bones are screened for lesions with x-rays or a CT scan.3
Bone marrow biopsy/aspiration. Bone marrow samples are critical to diagnose multiple myeloma, determine severity, and choose best treatments.5
Cytogenetic testing. These tests look for genetic abnormalities in bone marrow cells, including myeloma cells.5 Findings can help determine disease severity and guide treatment selection.2
Ms. Rummel: We need a bone marrow biopsy and other lab work to figure out what type of illness we’re dealing with. In the first 90 days, it’s all about getting a diagnosis, looking at the plasma cell count, looking at the genetics, and getting the patient started on an appropriate treatment.
Treatment Planning
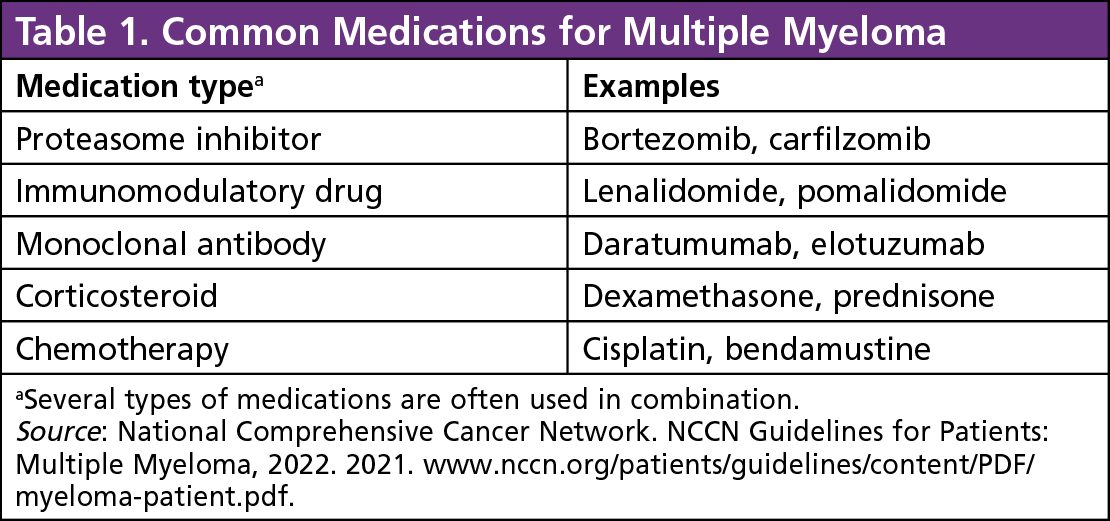
Over the past 2 decades, new therapies have significantly extended multiple myeloma survival.14 Whereas 2-drug combinations were previously the norm, almost two-thirds of patients now receive a 3-drug (triplet) regimen for first-line therapy.14 Recently, 4-drug combinations have been gaining ground and are recommended for certain patients with more aggressive disease.2 Table 1 provides an overview of common types of agents used to treat multiple myeloma, and examples of each.
Treatment selection first depends on type of disease. Unless a patient is participating in a clinical trial, MGUS is monitored without treatment, whereas smoldering myeloma may be treated if certain high-risk disease factors are present.2,12
Treatment options for active multiple myeloma are personalized based on a range of factors, including eligibility for autologous stem-cell transplant (ASCT; see Box), disease severity (risk level), and previous treatments.2 ASCT eligibility is typically determined by overall health, presence or absence of other health conditions, and age.2 Although the multiple myeloma landscape is rapidly changing, one thing will stay the same: treatment planning should always incorporate each patient’s personal values and goals, as these are essential factors in patient adherence to treatments and success.15
What Is Autologous Stem-Cell Transplant?
Because multiple myeloma and therapies for multiple myeloma can damage cells in the bone marrow, patients may undergo autologous stem-cell transplant to replace damaged cells. First, stem cells are harvested from the bone marrow. Next, remaining bone marrow cells (including cancer cells) are destroyed with chemotherapy. Finally, the patient’s stem cells are restored to the bone marrow, where they multiply and work again to create healthy blood and immune cells.3
Ms. Rummel: When reviewing specific treatment plans with patients, healthcare providers should focus on the basics, such as common side effects and number of treatment cycles. Together, patients, caregivers, and providers can figure out what treatment is going to work best.
Sticking with Therapy
Healthcare providers are aware that keeping up with multiple myeloma therapy can be challenging, so they have the knowledge and resources to help patients overcome obstacles, from the first 90 days and beyond.
Patient expectations are a key part of this process, because patients with realistic expectations more often take their therapy, experience fewer side effects, and maintain a better quality of life.16 Patients should consider asking how long therapy will last, and how long it will take to adjust to new medications. If concerns arise during treatment, rapid communication is essential, particularly if patients believe they are having side effects. Additional medical tests may be needed to determine if new symptoms are because of the medications or multiple myeloma itself.
Organization is also critical for sticking with therapy, especially for patients who are already taking other medications. Patients and their caregivers should consider using tools to organize the treatment process, including calendars, pill organizers and dispensers, and smartphone reminder apps.
Caregivers, family members, and friends can also offer key emotional support. Caregivers and loved ones should be aware that physical health is not always a good predictor of mental health, and that patients with multiple myeloma can feel down or anxious even when they are responding well to therapy, not needing therapy at all, or feeling physically well.17 At the same time, caregivers, family members, and friends can also be emotionally affected by a multiple myeloma diagnosis.18 These impacts can lead to a wide variety of issues, including disruptions in family organization and altered relationships.18 Social workers, therapists, and patient advocacy organizations may be needed to get through the tough times.
Ms. Rummel: Every patient is different, and things can change throughout the treatment journey. Maybe a patient starts working the night shift instead of a day shift, so we need to change their medication schedule so they can sleep. Sometimes it’s a simple fix; other times we need to be creative and think outside the box. Ultimately, patients are more likely to stick with therapy if they’re a part of the decision-making process, so it’s important for patients to know that they can help make decisions with their healthcare team. We always need to keep communication open.
Barriers to Care
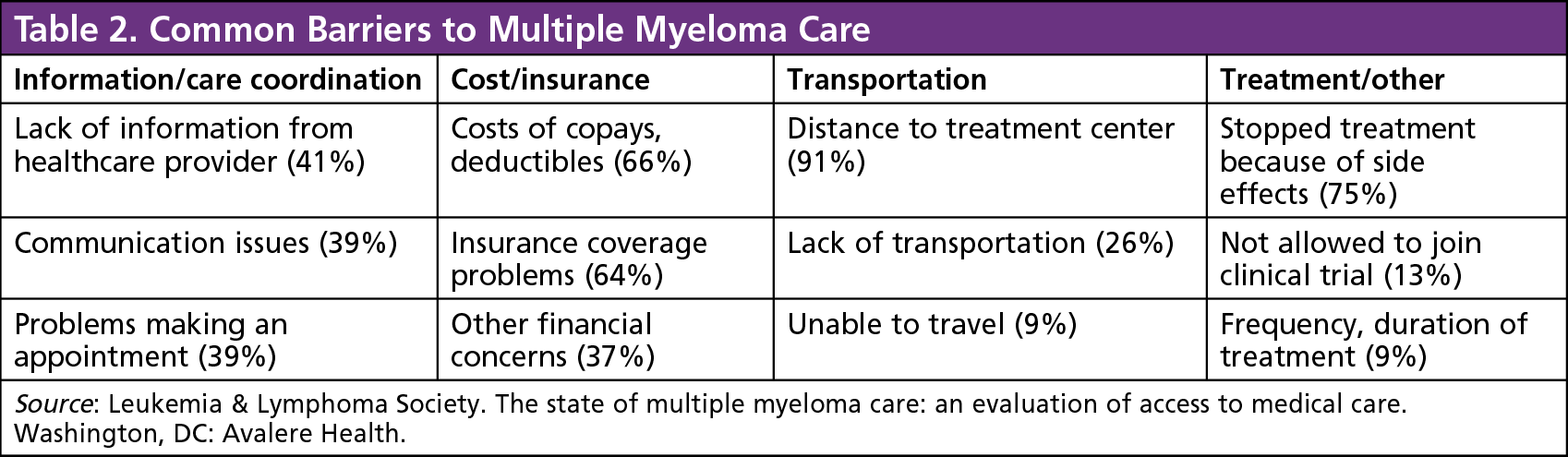
A recent survey of patients with multiple myeloma showed that 70% of patients encountered at least 1 barrier to care, and 37% of patients encountered 2 or more obstacles.7 These may include issues with information or care coordination, cost or insurance, transportation, and treatment itself. Table 2 shows the most common issues underlying these barriers. Although some obstacles cannot be fixed, such as a long distance between home and a treatment center, most of them can be addressed. For example, communication can be improved, which could in turn influence the rates of side effects, possibly improving chances of staying on therapy.16
To help find solutions, patients can turn to in-hospital support, including healthcare providers and social workers, as well as patient support organizations, such as the Leukemia & Lymphoma Society (LLS), CancerCare, the Patient Access Network Foundation, the International Myeloma Foundation (IMF), and others.19
Ms. Rummel: Patients and caregivers should have access to counseling or mental health services. If someone is newly diagnosed, they may not be coping well, or caregivers may not be coping well, and the situation can bring out old issues that need to be addressed for the patient and their caregiver to get through treatment. It’s important to be aware of the resources that are out there to help. Some of the supports are going to be different, depending on location, but the bigger resources that are out there, such as the LLS and the IMF, can help all patients.
Survivorship
Starting early in the treatment, patients need to prepare for their transition into posttreatment survivorship, a particularly important aspect of care for patients with multiple myeloma, who are living longer than ever before.20,21 According to the IMF Nurse Leadership Board, multiple myeloma survivorship plans should address 5 areas of concern: health maintenance, bone health, mobility and safety, renal health, and sexual health.22 If healthcare providers do not bring up these topics, patients and caregivers should feel empowered to open the conversation.
Ms. Rummel: Survivorship starts at the time of diagnosis. Patients don’t just stop treatment and go into survivorship. Once a patient is diagnosed, they become a survivor, and healthcare providers work with them through the cancer journey and its many ups and downs.
There’s a lot of information out there for patients, but it’s not all reliable. We don’t want patients pulling something out of nowhere and getting the wrong idea. Doctor Google is not an appropriate information source. Instead, patients should ask their healthcare provider about reliable, well-vetted information sources.
Conclusion
Over the past few decades, multiple myeloma survival has improved dramatically, largely as a result of the introduction of targeted therapies. Although better outcomes are cause for optimism, associated treatments and survivorship come with a new set of challenges.
Starting in the first 90 days, patients and providers need to consider medical and nonmedical factors, including possible barriers to care, common diagnostics, factors in therapy selection, strategies to take therapy as prescribed, and considerations for the posttreatment period. When all these factors are considered together, patients are more likely to have the best possible outcomes, from the first 90 days and beyond.
References
- Padala SA, Barsouk A, Barsouk A, et al. Epidemiology, staging, and management of multiple myeloma. Med Sci (Basel). 2021;9:3.
- Rajkumar SV, Kumar S. Multiple myeloma current treatment algorithms. Blood Cancer J. 2020;10:94.
- National Comprehensive Cancer Network. NCCN Guidelines for Patients: Multiple Myeloma, 2022. 2021. www.nccn.org/patients/guidelines/content/PDF/myeloma-patient.pdf.
- Dana-Farber Cancer Institute. Multiple myeloma: optimizing quality of life for survivors. Updated August 22, 2017. https://blog.dana-farber.org/insight/2017/08/multiple-myeloma-optimizing-quality-of-life-for-survivors. Accessed April 9, 2020.
- American Cancer Society. Multiple myeloma early detection, diagnosis, and staging. www.cancer.org/cancer/multiple-myeloma/detection-diagnosis-staging.html.
- Gupta S, Abouzaid S, Liebert R, et al. Assessing the effect of adherence on patient-reported outcomes and out of pocket costs among patients with multiple myeloma. Clin Lymphoma Myeloma Leuk. 2018;18:210-218.
- Leukemia & Lymphoma Society. The state of multiple myeloma care: an evaluation of access to medical care. Washington, DC: Avalere Health.
- Solano M, Daguindau E, Faure C, et al. Oral therapy adherence and satisfaction in patients with multiple myeloma. Ann Hematol. 2021;100:1803-1813.
- Korde N, Kristinsson SY, Landgren O. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM): novel biological insights and development of early treatment strategies. Blood. 2011;117:5573-5581.
- Landgren O, Kyle RA, Rajkumar SV. From myeloma precursor disease to multiple myeloma: new diagnostic concepts and opportunities for early intervention. Clin Cancer Res. 2011;17:1243-1252.
- Muchtar E, Kumar SK, Magen H, Gertz MA. Diagnosis and management of smoldering multiple myeloma: the razor’s edge between clonality and cancer. Leuk Lymphoma. 2018;59:288-299.
- International Myeloma Foundation. What are MGUS, smoldering multiple myeloma, and active myeloma? www.myeloma.org/what-are-mgus-smm-mm.
- Tosi P, Tomassetti S, Merli A, Polli V. Serum free light-chain assay for the detection and monitoring of multiple myeloma and related conditions. Ther Adv Hematol. 2013;4:37-41.
- Braunlin M, Belani R, Buchanan J, et al. Trends in the multiple myeloma treatment landscape and survival: a U.S. analysis using 2011-2019 oncology clinic electronic health record data. Leuk Lymphoma. 2021;62:377-386.
- Glatzer M, Panje CM, Sirén C, et al. Decision making criteria in oncology. Oncology. 2020;98:370-378.
- Nestoriuc Y, von Blanckenburg P, Schuricht F, et al. Is it best to expect the worst? Influence of patients’ side-effect expectations on endocrine treatment outcome in a 2-year prospective clinical cohort study. Ann Oncol. 2016;27:1909-1915.
- Maatouk I, He S, Hummel M, et al. Patients with precursor disease exhibit similar psychological distress and mental HRQOL as patients with active myeloma. Blood Cancer J. 2019;9:9.
- Gorman LM. Psychosocial impact of cancer on the individual, family, and society. In: Bush NJ, Gorman L, eds. Psychosocial Nursing Care Along the Cancer Continuum. 3rd ed. Pittsburgh, PA: Oncology Nursing Society; 2018:3-26.
- Natale N. Multiple myeloma resources. Everyday Health. Updated July 29, 2021. www.everydayhealth.com/multiple-myeloma/guide/resources. Accessed September 21, 2021.
- Baileys K, McMullen L, Lubejko B, et al. Nurse navigator core competencies: an update to reflect the evolution of the role. Clin J Oncol Nurs. 2018;22:272-281.
- Daudt HML, van Mossel C, Dennis DL, et al. Survivorship care plans: a work in progress. Curr Oncol. 2014;21:e466-e479.
- Bilotti E, Faiman BM, Richards TA, et al. Survivorship care guidelines for patients living with multiple myeloma: consensus statements of the International Myeloma Foundation Nurse Leadership Board. Clin J Oncol Nurs. 2011;15(suppl):5-8.
Read Letter to the Editor Thank You CONQUER Magazine for a Great Article