To download this article as a PDF, see the link below.
CPS1423
Promising medical advances are changing how oncologists and surgeons treat people with lung cancer. Learning that you or a family member has lung cancer can be overwhelming, but there is more hope today than ever before. Treatment plans can now be customized, or personalized, to each patient’s specific subtype of lung cancer, with the goal of extending survival and potentially enhancing quality of life.
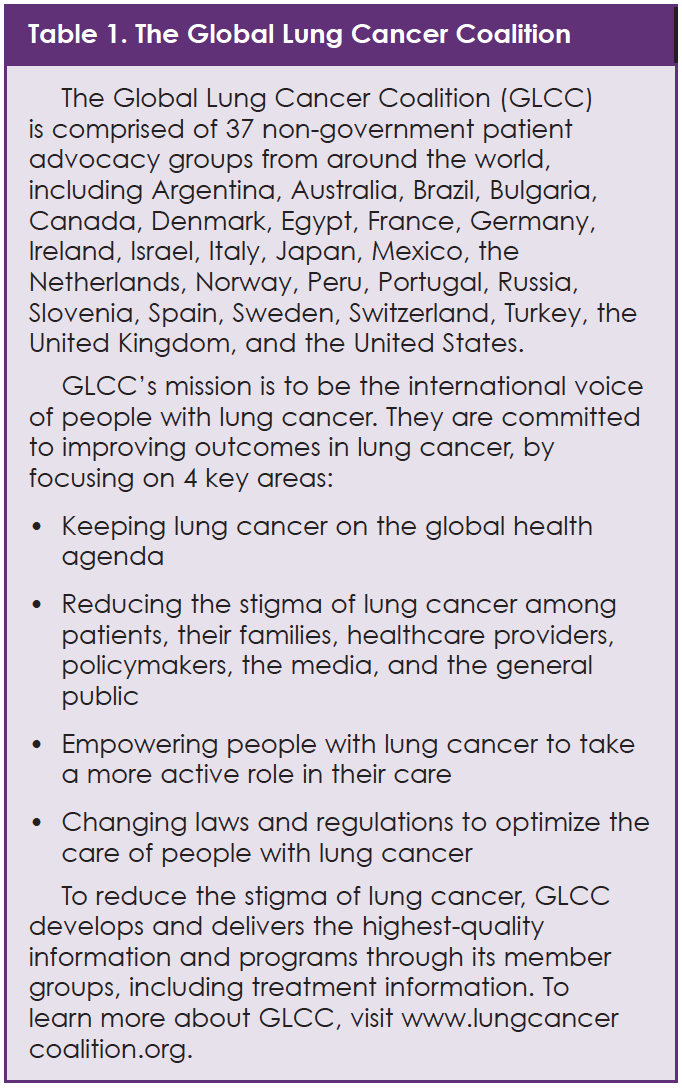
This article reviews key developments in the diagnosis and treatment of patients with lung cancer, with a focus on the importance of biomarker testing. It will provide patients with the knowledge to help them partner with their medical team to ensure treatment plans are tailored to them. Much of the information, ideas, and recommendations in this article come from a group of global lung cancer patient advocacy experts who are affiliated with the Global Lung Cancer Coalition (GLCC), an alliance of patient organizations that is committed to increasing the understanding of lung cancer and improving lung cancer outcomes for patients (see Table 1).
In February 2018, experts from the United States, Canada, Mexico, Indonesia, and the European Union met in Cambridge, Massachusetts, to take part in the GLCC Roundtable, which was sponsored by Takeda Oncology. Roundtable participants talked about the unique needs of patients with lung cancer; difficulties associated with access to biomarker testing throughout the world; and the value of using biomarker test results when making treatment decisions.
This article is organized into 3 parts. The first part reviews lung cancer and its various subtypes, as well as types of biomarker tests and why they are important. The second part highlights insights and ideas from the GLCC Roundtable participants regarding patient education and access to lung cancer care around the world. The final part provides practical advice for patients who have been diagnosed with lung cancer and their caregivers about how to engage with their healthcare team regarding biomarker testing and treatment choices.
Part I. Lung Cancer and the Importance of Biomarker Testing
Lung cancer begins when abnormal cells in the lung grow out of control. However, the term “lung cancer” is very broad. There are several stages and forms (or subtypes) of lung cancer. Lung cancer may behave in different ways in different people, depending on factors such as its stage and subtype.1
Stages of Lung Cancer
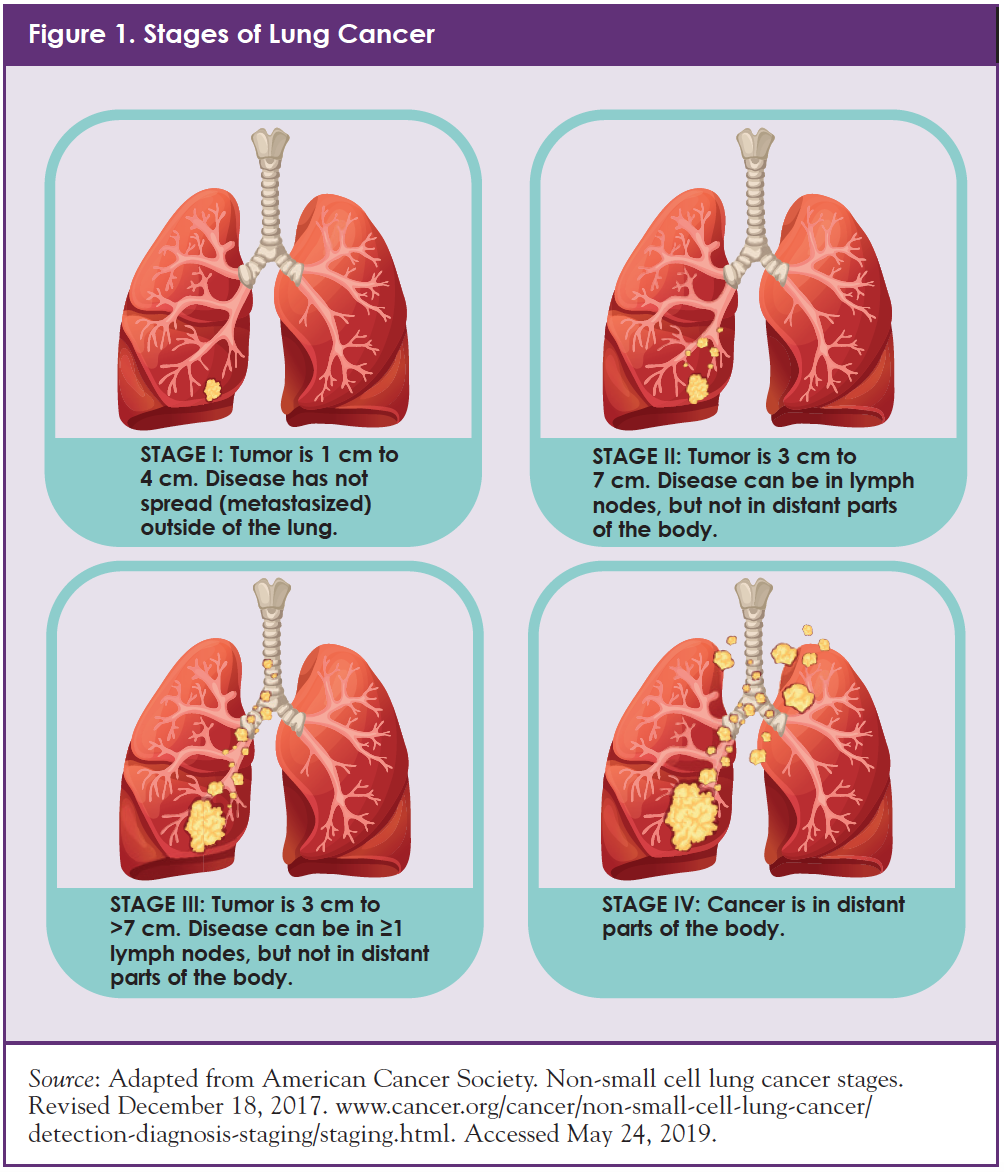
When lung cancer is diagnosed and treated at an early stage (before it spreads), chances of treatment success are higher than in later stages. Therefore, when oncologists “stage” a patient’s cancer, they want to learn if and how far the cancer has spread from its original source. Figure 1 shows the 4 main stages of lung cancer2:
- Stage I: Cancer is in the lung only; it has not spread outside the lung
- Stage II: Cancer is in the lung and lymph nodes inside the lung
- Stage III: Cancer is in the lung and lymph nodes outside the lung
- Stage IV: Cancer has spread to both lungs, the area around the lungs, and/or to distant organs, such as liver, bones, or brain
Oncologists and surgeons use information about lung cancer stages to help decide which treatments—surgery, radiation, chemotherapy, or other targeted cancer drugs—are most appropriate.2,3
Subtypes of Lung Cancer
As oncologists, surgeons, and other cancer care providers develop treatment plans for patients with lung cancer, knowledge is power. The more they learn about the specific makeup of the patient’s tumor, the greater the chance that they will be able to target the cancer with a specific type of treatment.1,3
This means that, in addition to staging the patient’s lung cancer based on its size, location, and spread, doctors also take a sample of the lung cancer tissue itself.1 Tissue from the patient’s lung is typically obtained through a biopsy or after surgical removal (or resection) of the tumor.
Remember that lung cancer is not one disease. There are different types (subtypes) of lung cancer, and each behaves in a different way.1 Oncologists use sophisticated tumor testing to identify the specific category or subtype of the patient’s lung cancer, which helps them to make the best decisions about treatment.1
There are 2 main types of lung cancer based on the size, shape, and look of the cancer cells under a microscope: (1) small-cell lung cancer and (2) non–small-cell lung cancer (NSCLC). About 85% of people with lung cancer have NSCLC.4
NSCLC also has several subcategories. To learn which subcategory of NSCLC a patient has, physicians perform 2 types of tests: pathology (or tissue structure) testing and biomarker testing.1
Pathology tests are performed by physicians who look at the histology (appearance) of NSCLC cells through a microscope. These physicians (pathologists) are experts in cancer diagnosis. They focus on the size and shape of the cells to learn if the patient has squamous NSCLC (about 30%) or non-squamous NSCLC (about 70%).4 Non-squamous NSCLC includes “adenocarcinoma” and “large-cell” cancers.4
Squamous NSCLC begins in the thin flat cells that line the passages of the respiratory tract.4,5 It is often linked to a history of smoking and tends to be found in the center of the lungs, near a main airway or bronchus.5,6
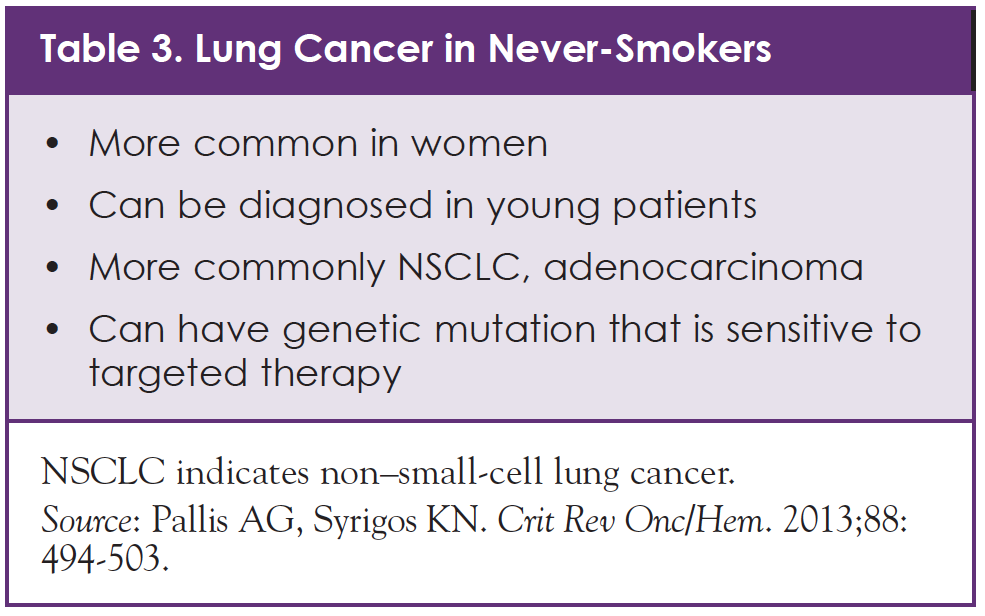
Adenocarcinoma, the most common subtype of NSCLC, begins in the cells that form the lining of the lungs.4,6 Adenocarcinoma is more common in women than in men, and is more common in never-smokers.6,7 Each of these subtypes of NSCLC behaves differently and has a different expected outcome or prognosis.6
Biomarker Testing in NSCLC
Scientific advances over the past several years have allowed cancer specialists to obtain more detailed and accurate information to help them to personalize therapy to each patient. In addition to learning NSCLC histology—squamous or non-squamous—cancer specialists also test for NSCLC biomarkers.1
A biomarker is a biological molecule found in blood, other body fluids, or tissues that is a sign of a normal or abnormal process, or of a condition or disease.8 Biomarkers are used to see how well the body responds to a treatment for a disease or condition. For patients with lung cancer, biomarker tests can look for specific features. After the pathologist shares biomarker findings with oncologists, the team can consider use of targeted treatments that may have higher chances of success.1,9
It is important to understand that the language that cancer specialists use to talk about biomarker testing can vary from one specialist to another. “Biomarker testing,” “molecular testing,” and “genetic testing” are essentially the same. Oncologists and other medical specialists often use these terms interchangeably.9
Gene mutations are one type of biomarker. These are changes that occur in a cell’s genetic “blueprint” or DNA (Table 2).9-11 DNA gives our cells instructions about how to behave, including how to divide and grow.9-11 DNA also tells cells which proteins (or essential complex biological compounds) they should make.9 This means that protein levels can be another type of biomarker.9 For example, people with prostate cancer can have high levels of lactate dehydrogenase (LDH) in their blood. Blood tests can show whether these LDH levels drop during cancer treatment, which helps doctors and patients learn if the cancer treatment is working.
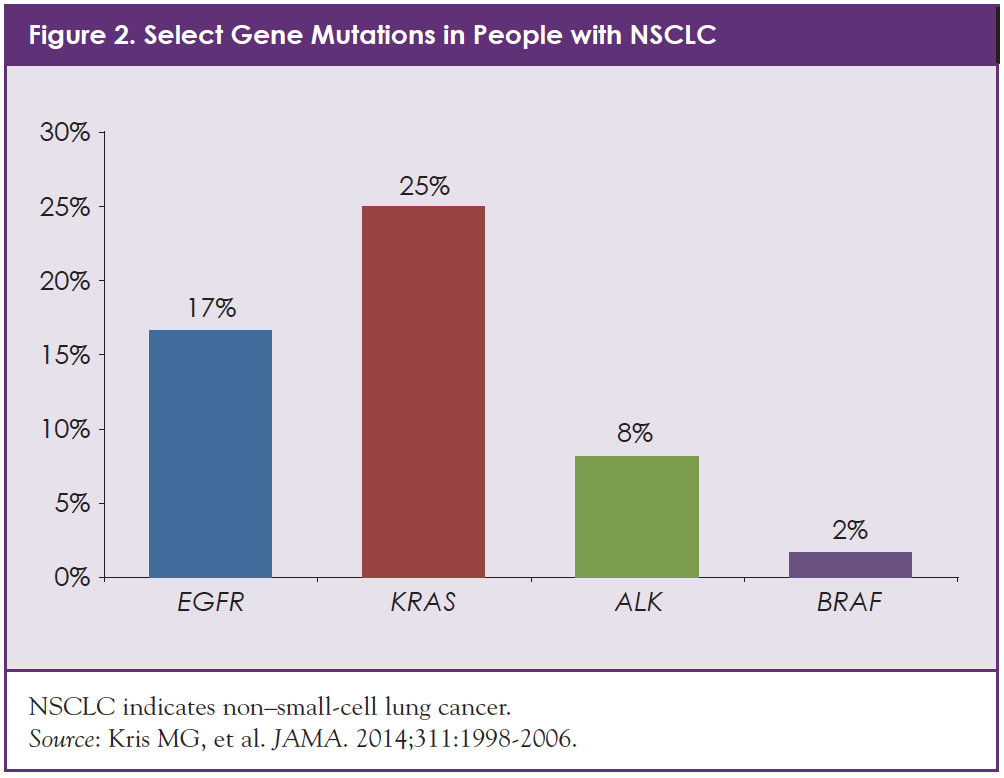
Patients with NSCLC may also be tested for PD-L1, a protein that may help determine whether a patient’s tumor will respond well to certain immunotherapy drugs.1 Figure 2 shows some of the specific gene mutations that have been identified in people with NSCLC.12 Some of the most common gene mutations identified in NSCLC are called EGFR, ALK, ROS1, and BRAF.1
Why Test for NSCLC Mutations and Other Biomarkers?
Today, more than 75% of patients with NSCLC, specifically adenocarcinomas, have genetic alterations that oncologists may be able to target with one or more available drug therapies that can address an identified mutation.3 For other patients with NSCLC whose genetic mutations do not yet have approved treatments, ongoing scientific research is dedicated to finding effective treatment options.
A common mutation in NSCLC can occur in the gene that controls the epidermal growth factor receptor (EGFR).1 EGFR is a protein that is found on the surface of cells in the body, including cancer cells. If the EGFR gene is mutated, EGFR proteins on the cell surface become overactive and cause cancer cells to grow quickly.13
Patients whose cancer cells have a mutated EGFR gene, meaning their cancer cells make too much EGFR protein, have what oncologists call “EGFR-positive” NSCLC. Drugs known as EGFR inhibitors (or blockers) have been approved by the US Food and Drug Administration, the European Medicines Agency, and other regulatory agencies worldwide, and can be offered to patients with EGFR-positive NSCLC.
In other types of NSCLC, cancer growth is caused in part by a rearrangement in the anaplastic lymphoma kinase (ALK) gene.1 Gene rearrangement means that one gene has fused with another gene to create a new gene. In some lung cancers, the ALK gene fuses with the EML4 gene. This EML4-ALK fusion gene, which is seen in about 8% of patients with NSCLC, results in an overactive ALK protein that can drive cancer-cell growth.12
In the United States, testing for ALK and lesser known mutations is recommended for all patients with NSCLC that has spread to other parts of the body (metastatic NSCLC), including adenocarcinoma, large-cell lung carcinomas, and unknown subtypes.1 Non-smokers or light smokers who have the adenocarcinoma subtype of NSCLC are more likely to have “ALK-positive” NSCLC (or NSCLC with ALK mutation).13 Drugs called ALK inhibitors are available in the United States and in Europe, as well as in other areas of the world, and are an option for patients with ALK mutation.
Lung Cancer Diagnosis in Non-Smokers
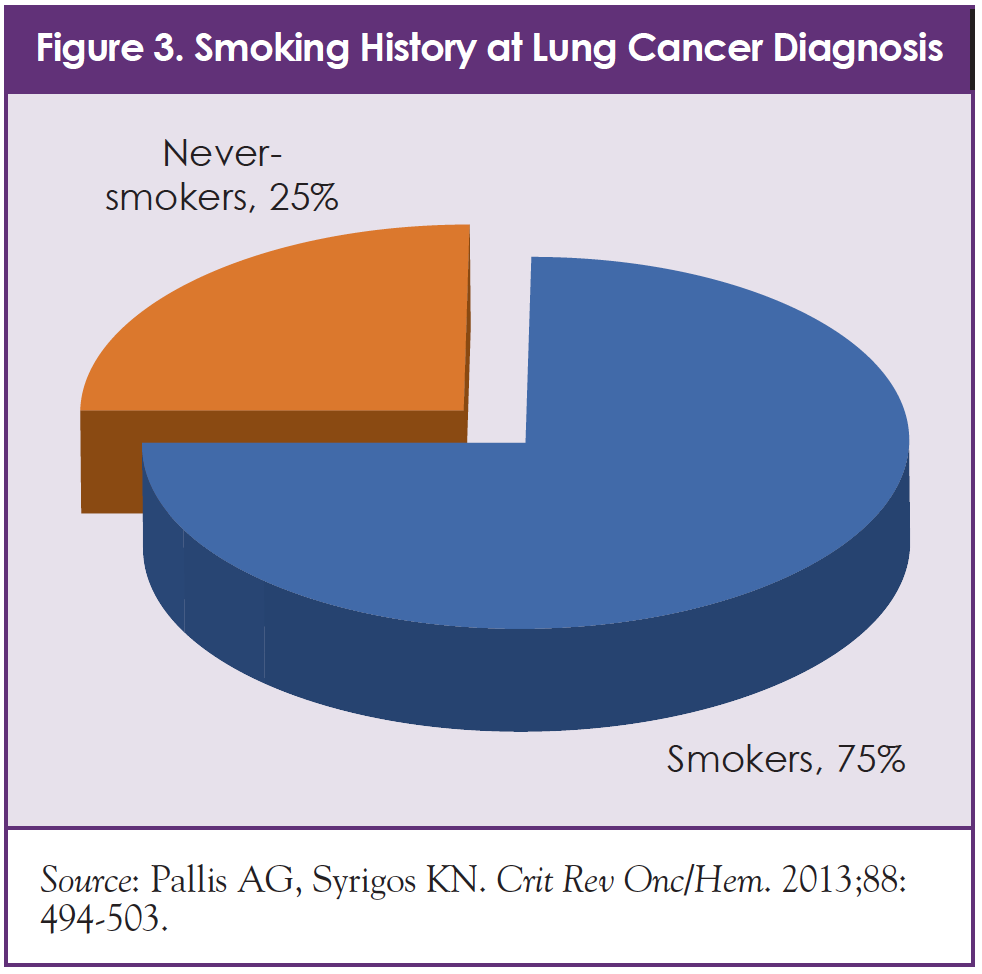
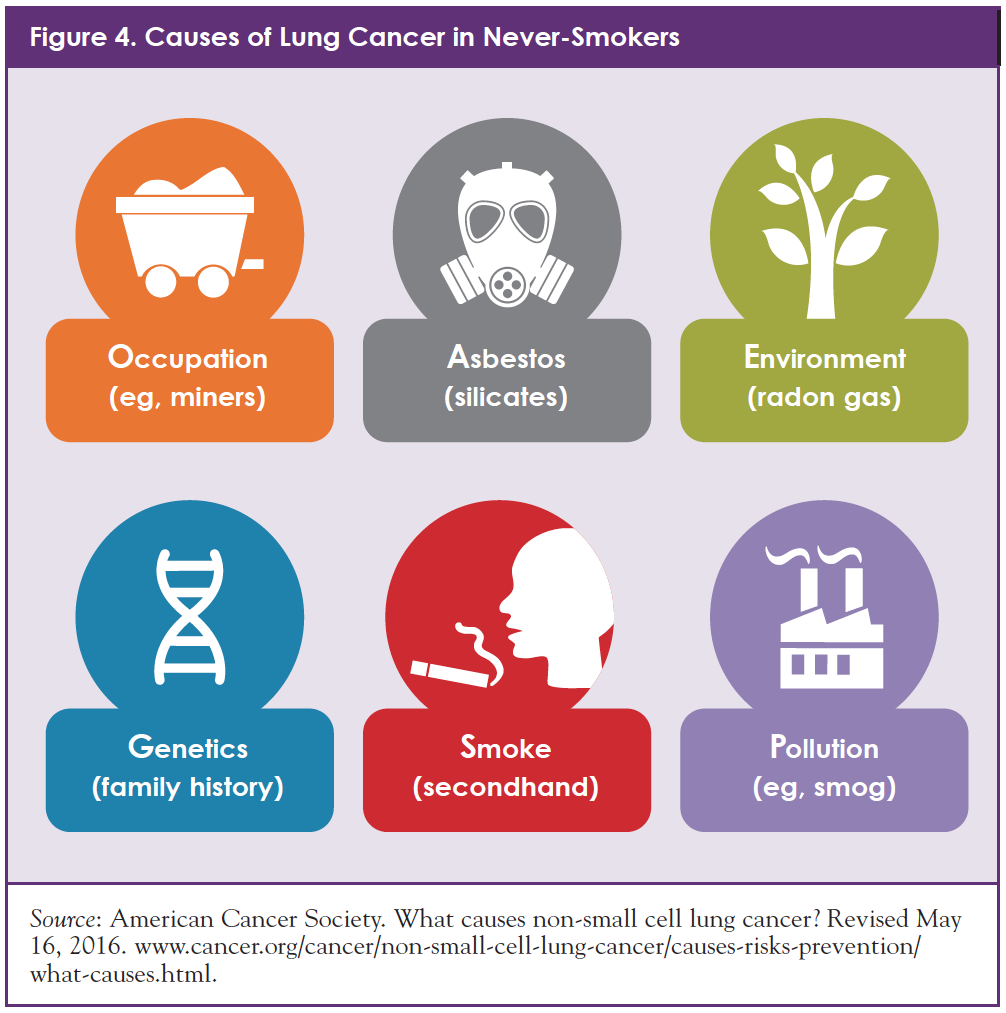
Approximately 25% of people who are diagnosed with lung cancer have never smoked (Figure 3).14 For these patients, different factors, such as genetic vulnerability and exposure to cancer-causing chemicals (such as secondhand smoke, air pollution, radon, or asbestos) can be a driver of disease (Figure 4).15 In other patients, NSCLC occurs without a known cause.15
Lung cancer in non-smokers can be different from lung cancer in people who smoke (Table 3).14 Non-smokers who are diagnosed with NSCLC tend to be diagnosed at a younger age and may have certain genetic changes, including ALK and EGFR mutations.13-15
Treatments That Target NSCLC Subtypes
Doctors use many types of treatments for patients with lung cancer, including radiation, surgery, and medications such as chemotherapy drugs. Although effective for many patients, these treatments can be tough to tolerate, in part because they often destroy normal healthy cells in the process of destroying cancer cells. Today, with a more complete understanding of how cancer cells behave, researchers have developed medications that target specific genetic changes in NSCLC, including specific mutations and abnormal proteins.1
The medical community now understands that by blocking certain internal communications or signaling pathways in cancer cells, growth of these cells can be slowed or stopped. Using this knowledge, unique drugs have been developed that can block or “inhibit” specific cancer-cell signaling pathways. As a group, these drugs are called “targeted” therapies.1 This means that some patients with NSCLC (and some patients with other kinds of cancer) can now be treated in more precise ways. This idea is sometimes referred to as “personalized” medicine. The concept of personalized medicine means that physicians use the right treatment, for the right disease, in the right patient, and at the right time.16 For example, people with ALK-positive NSCLC may be treated with an ALK inhibitor. Similarly, those with EGFR-positive NSCLC may be treated with an EGFR inhibitor.
Part II. Insights and Ideas from the GLCC Roundtable Meeting
The GLCC is a coalition of patient organizations that is committed to increasing the understanding of lung cancer and improving lung cancer outcomes. Sponsored by Takeda Oncology, the GLCC Roundtable focused on the needs of patients with lung cancer; challenges associated with access to biomarker testing throughout the world; and the use of biomarker test results to make treatment decisions. Selected topics that these doctors and patient advocates discussed are highlighted below.
Pre-Habilitation
What happens when patients are “in between” their NSCLC diagnosis and the start of treatment? After diagnosis, they often have appointments with various doctors. They may also need to go to imaging centers for scans, as well as laboratories for blood work. However, waiting for these test results prior to starting treatment for cancer—which can take days to weeks—can be challenging. Many people with NSCLC feel a sense of urgency to start treatment. However, knowing the important role that targeted therapies can play in people with metastatic NSCLC, cancer specialists may want to wait until all biomarker tests are complete. This should, of course, be a conversation between the patient and the doctor to make the appropriate decision.
To make this waiting time as productive and meaningful as possible for patients and their caregivers, experts are developing pre-habilitation programs. “Pre-habilitation” refers to educational programs that help patients and their caregivers learn more about NSCLC, prepare mentally and physically for treatment, and plan their cancer journey—pre- and post-treatment.17
GLCC Roundtable members explained that in some countries, “pre-habilitation” programs help patients and caregivers to improve their nutrition, reduce stress, exercise, stop smoking (if relevant), and handle logistics, such as travel arrangements, childcare planning, work-related communications, and insurance paperwork. Patients may also have the chance to connect with one or more of their cancer care team members, including oncologists, surgeons, nurses, financial counselors, nutritionists, psychologists, and other healthcare professionals, as well as peer mentors where available.18 “Some patients may think about seeking the best doctor, but with pre-habilitation, they are building the best network,” said Dr. Johannes Bruns, from Germany.
Programs such as these are being developed in the United States and in other countries around the world. In the United States, for example, nurses and nurse navigators have become central to the care of patients with cancer and their families.17 Navigators are healthcare professionals—often nurses—who guide patients through the many confusing steps associated with a cancer diagnosis, testing, and treatment. They typically accompany the patient through their cancer journey.
GLCC Roundtable participant Winfield Boerckel, Lung Cancer Program Coordinator at Long Island CancerCare, reinforced the critical role of caregivers in the pre-habilitation team. He reminded the group that caregivers often ask the treatment team questions about issues that patients may be reluctant to talk about. Caregivers can also be better notetakers and “reporters” of complex information since patients may experience overwhelming emotions during this time. In many families, caregivers serve as a “translator” of complex information. Caregivers often see the situation from a different perspective, although they are intimately involved with the patient and his or her NSCLC experience.
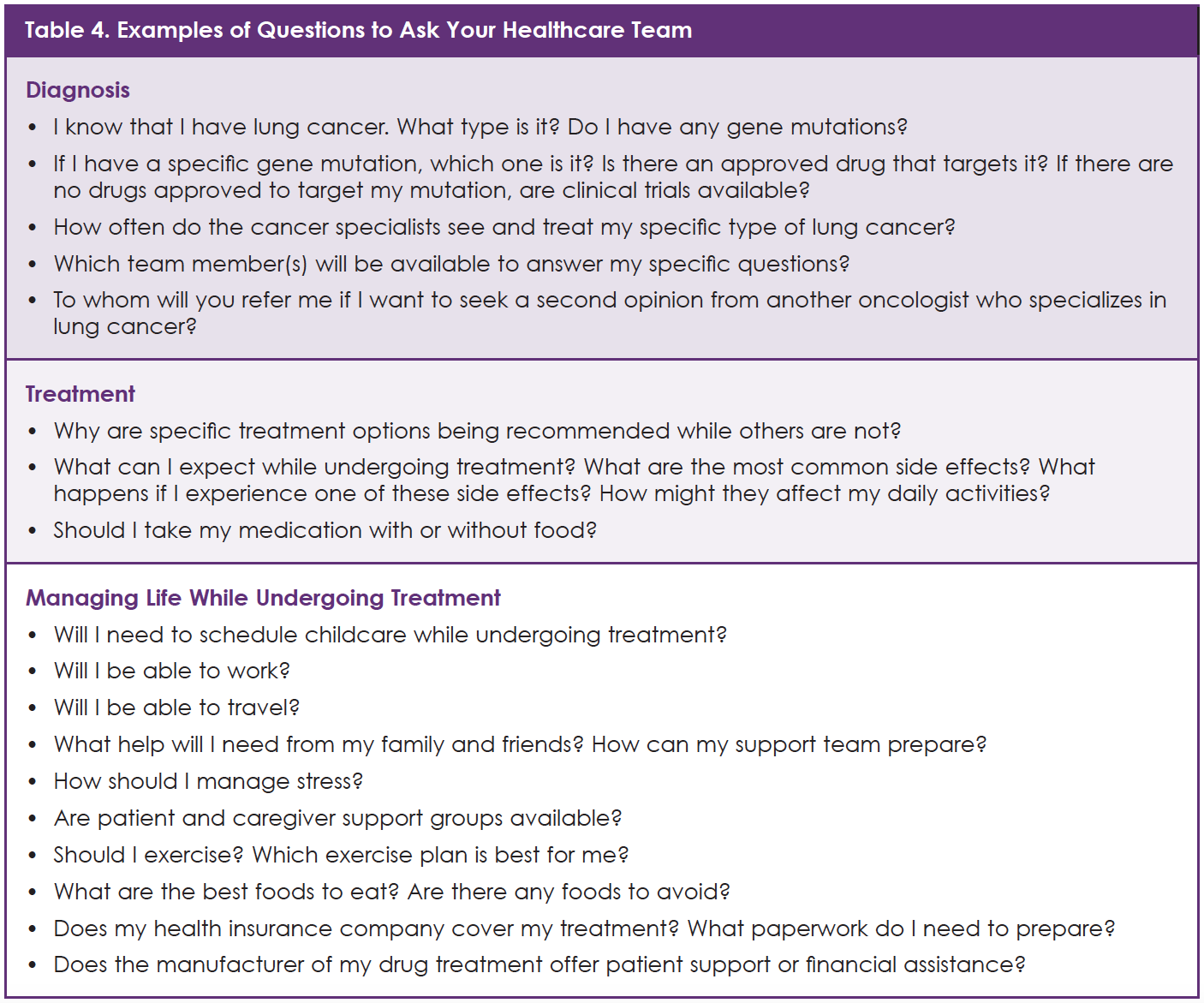
If you are diagnosed with NSCLC or are a caregiver for someone with lung cancer who does not have access to a pre-habilitation program, you may want to use the questions listed in Table 4 to help create your own pre-habilitation approach.
Accessing Biomarker Testing in NSCLC
Members of the GLCC Roundtable explained that biomarker testing is not performed routinely for many patients with NSCLC; it is not a standard practice around the world. These patient advocates described how the rate of testing for EGFR and ALK mutations varies across countries, as well as among cancer care systems within each country.19
In some parts of the world, patients’ ability to be tested for NSCLC biomarkers is limited by availability and cost. Patricia Mondragón, President and Cofounder of Respirando con Valor (Breathing Bravely), an advocacy association for patients with lung cancer and their families based in Mexico City, explained, “Outside of the main cancer institutions in Mexico, you cannot really get access to NSCLC tests. And, if patients do have access, many cannot afford the testing.”
Another GLCC Roundtable participant, Adityawati Ganggaiswari, of the Indonesian Cancer Foundation, a non-governmental organization in Jakarta, Indonesia, said, “In my country, access to testing depends on the particular doctor and on restrictions from insurance companies. Unless patients go onto a clinical trial, they might not get access to molecular testing.”
How can these challenges be addressed so that all patients with NSCLC can be tested and learn whether they are candidates for newer targeted treatments? GLCC Roundtable participants shared their experiences.
Mr. Boerckel added, “Patients are not always told what to expect in terms of scans, blood work, and biomarker testing. We believe that it is important for patients to be informed partners in their care decisions.”
Another GLCC Roundtable participant, Jesme Fox, of the Roy Castle Lung Cancer Foundation in the United Kingdom, reminded the group how important it is for all parties involved in NSCLC care to coordinate with each other. “All stakeholders—pulmonologists, oncologists, pathologists, patients, and advocacy groups—need to work together to improve rates of biomarker testing,” Dr. Fox said.
Patient advocacy groups and coalitions such as the GLCC are committed to educating patients with lung cancer about the disease and its management, including the importance of biomarker testing. These organizations drive needed change through government policy initiatives and educational programs. The doctors and patient advocates affiliated with these organizations are committed to improving care for patients with lung cancer.
Part III. Partnering with Your Medical Team
If you have been diagnosed with NSCLC, or you care for someone who has been diagnosed, you know that there are many sources of information and advice. This section is designed to help you talk with your healthcare team about biomarker testing and the impact of test results on your treatment choices. To identify the key people who are involved in this aspect of your care, a sports team analogy fits: Who are your coaches? Who is on the field? Who is on the bench? What role does each person play in team decision-making?
Cancer Doctors: Pulmonologists, Radiation Oncologists, Thoracic Surgeons, Medical Oncologists, and Pathologists
Doctors lead a medical team like a coach leads a baseball or a football team. Five types of doctors are likely to be directly involved in the care of patients with NSCLC.18
Pulmonologists diagnose and treat various types of lung disease, such as emphysema, COPD (chronic obstructive pulmonary disease), asthma, and cancer of the lung. A pulmonologist can be the doctor who requests biopsies, blood work, and biomarker tests, and he or she will treat patients who have breathing issues related to lung cancer.18
Radiation oncologists are physicians who use radiation therapy to treat cancer. Radiation oncology is 1 of the 3 primary specialties involved in the treatment of cancer, in addition to surgical oncology and medical oncology.
Thoracic surgeons are doctors who perform surgery on organs inside the thorax or the chest. Some thoracic surgeons treat patients with heart disease, while others focus on patients with lung disease. Some thoracic surgeons have specialized training in surgical oncology, which is the use of surgical techniques to remove cancer that is in and around the lung.18
Medical oncologists are physicians who specialize in treating cancer. Some medical oncologists have specific expertise in lung cancer, such that they are called “thoracic oncologists.” The medical oncologist is often considered your head coach; he or she directs your care and taps into the different types of doctors who are sitting on your “bench.” This means that the oncologist makes referrals to other specialists who might help you, such as radiation oncologists (cancer doctors who administer radiation therapy), surgical oncologists (cancer doctors who perform surgery), pain management specialists, psychiatrists, nutritionists, and physical therapists.18
Pathologists are critical players on the team. These doctors use microscopes and other more sophisticated equipment to examine tissue samples (cancer cells) from your lung. Like a detective, the pathologist’s job is to determine if a patient has lung cancer, as well as the type of lung cancer and (working with the medical oncologist) the cancer stage. In this detective role, pathologists are responsible for biomarker testing for each patient with lung cancer. The pathologist then shares test findings with the care team so that the medical oncologist and other team members can determine the best course of personalized treatment for the patient.18
Because pathologists are on the front lines of testing, they are often the first to learn that a patient with NSCLC has a specific genetic mutation, such as EGFR or ALK. Pathologists are trained to recognize that certain features, including sex, age, and smoking status, can indicate that a patient with NSCLC is more or less likely to have a certain mutation. This can mean that this patient is more or less likely to benefit from a novel targeted treatment.1 For example, when a woman aged <40 years who has never smoked is found to have lung cancer, the pathologist may suspect that certain mutations are present, such as ALK.14 These suspicions prompt the pathologist to run appropriate tests and talk to the patient’s medical oncologist about implications for treatment.
Patients, Family Members, Caregivers, and Advocates
The patient is at the center of the care team, whereas doctors and other healthcare professionals, including caregivers, all work to do their best for the patient. Like all of the other team members, patients should consider taking an active role in training—learning about the disease and the treatments—and discussing each step along the way with their doctors, including testing and treatment decisions.
Because a lot of information is accessible online, patients and their families often start there as they seek knowledge. Understandably, patients want to know more about NSCLC and make connections with other people with lung cancer. During this exploration, patients and caregivers may also discover information about mutation and biomarker testing that helps them to ask good questions of their oncologists, understand test results, and appreciate the implications of these results for treatment.
NSCLC developments happen at a fast pace, which means that patients and families need information that is up-to-date, clear, and accurate. The information, whether it is found online or in a local library, should be reported by trustworthy sources. Patients should talk with their cancer care team and ask questions about the information they find.
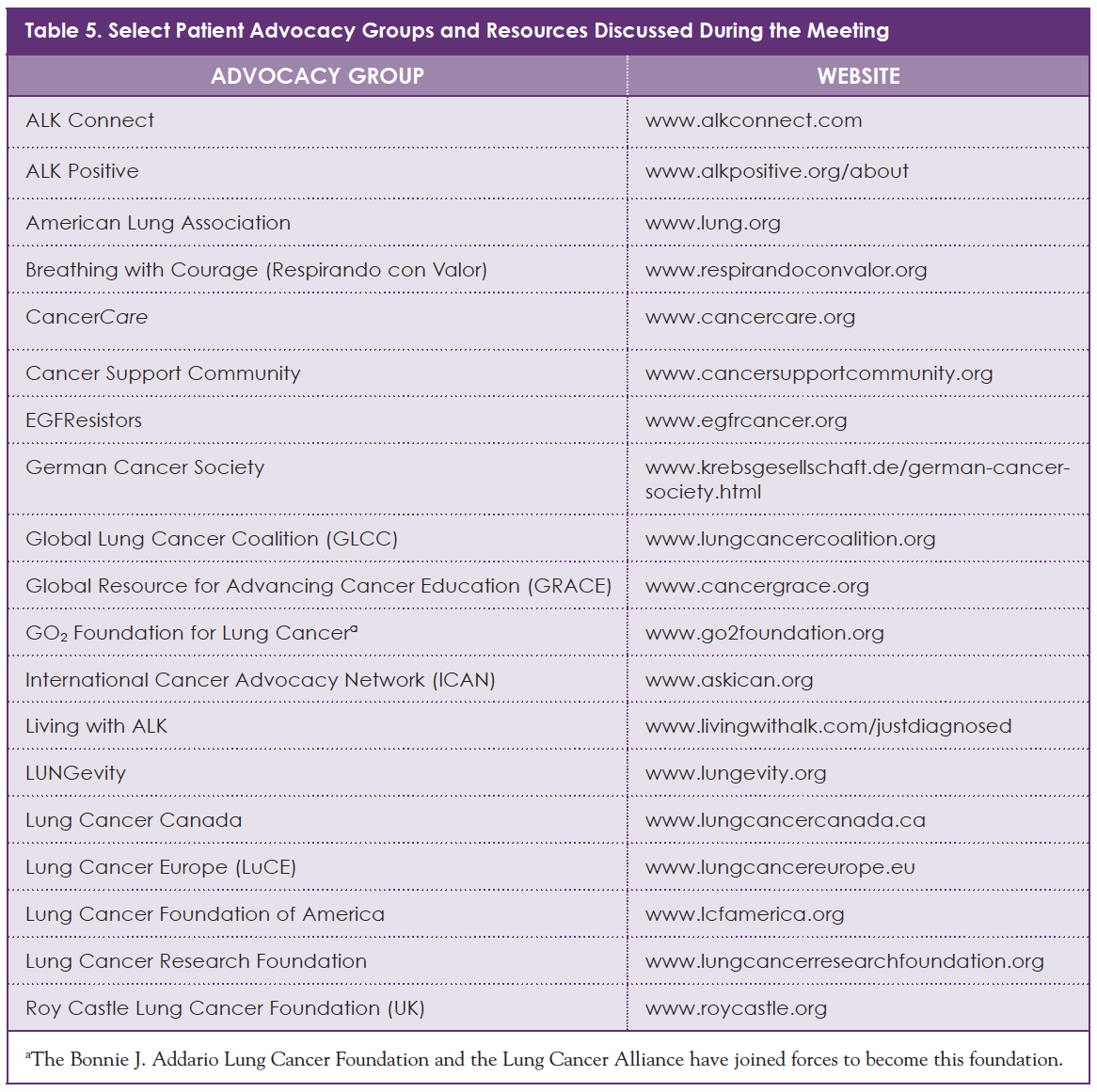
Today, many trusted patient advocacy groups provide online resources and support for people with cancer. As shown in Table 5, some of these groups, including GLCC, focus specifically on lung cancer, whereas others are devoted to patients with specific subtypes of lung cancer, such as people who have ALK-positive NSCLC. As with many illnesses that affect a small number of people, patients and caregivers look to each other for information, empathy, and support. Their shared experiences are often a great comfort when you are dealing with a potentially life-threatening illness.
If you are diagnosed with lung cancer, you should learn whether your cancer involves specific mutations, including ALK, EGFR, or others that make you eligible for targeted medicines. You can empower yourself by taking an active role in your care, asking questions, and talking with your cancer care team about each decision.
Consider seeking second opinions to learn whether your team has considered all treatment options for you. Patients and caregivers should not hesitate to learn more from their cancer care team and the larger cancer community about these and all other aspects of cancer care. Your doctors, nurses, and everyone who supports you are striving to offer the best care possible.
As our understanding of NSCLC continues to evolve, research and new developments offer greater hope to patients and their families. Today, patients with NSCLC and their families and caregivers have access to many valuable resources and support, as well as more effective and personalized treatment options. By learning about the role of tumor testing, including biomarker testing, for determining treatment options, patients can work even more effectively with medical specialists. Patients today can navigate an NSCLC diagnosis with more confidence and self-determination than ever before.
References
- American Lung Association. What you need to know about lung cancer tumor testing. November 2018. www.lung.org/assets/documents/lung-health/what-you-need-to-know-about-tumor-testing.pdf. Accessed May 24, 2019.
- American Cancer Society. Non-small cell lung cancer stages. Revised December 18, 2017. http://www.cancer.org/cancer/non-small-cell-lung-cancer/detection-diagnosis-staging/staging.html. Accessed May 24, 2019.
- Mendes E. Discovery of new lung cancer mutations may mean more treatment options. July 25, 2014. www.cancer.org/latest-news/discovery-of-new-lung-cancer-mutations-may-mean-more-treatment-options.html. Accessed May 24, 2019.
- Lung Cancer Alliance. Types of lung cancer. https://lungcanceralliance.org/what-is-lung-cancer/types-of-lung-cancer/. Accessed May 24, 2019.
- American Cancer Society. What is non-small cell lung cancer? Revised May 16, 2016. www.cancer.org/cancer/non-small-cell-lung-cancer/about/what-is-non-small-cell-lung-cancer.html. Accessed July 11, 2019.
- Lung Cancer Research Foundation. Non-Small Cell Lung Cancer. www.lungcancerresearchfoundation.org/lung-cancer/non-small-cell-lung-cancer. Accessed May 24, 2019.
- Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med. 2011;32:605-644.
- National Cancer Institute. NCI Dictionary of Cancer Terms. www.cancer.gov/publications/dictionaries/cancer-terms/def/biomarker. Accessed June 6, 2019.
- LUNGevity. What you need to know about biomarker testing. www.lungevity.org/sites/default/files/file-uploads/biomarker-testing-brochure-110617.pdf. Accessed July 31, 2019.
- American Cancer Society. Glossary: definitions & phonetic pronunciations. www.cancer.org/cancer/glossary.html. Accessed May 22, 2019.
- National Institutes of Health. Genetics Home Reference. What is a gene mutation and how do mutations occur? https://ghr.nlm.nih.gov/primer/mutationsanddisorders/genemutation. Accessed May 26, 2019.
- Kris MG, Johnson BE, Berry LD, et al. Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA. 2014;311: 1998-2006.
- American Cancer Society. Targeted therapy drugs for non-small cell lung cancer. Revised November 5, 2018. www.cancer.org/cancer/non-small-cell-lung-cancer/treating/targeted-therapies.html. Accessed May 26, 2019.
- Pallis AG, Syrigos KN. Lung cancer in never smokers: disease characteristics and risk factors. Crit Rev Onc/Hem. 2013;88:494-503.
- American Cancer Society. What causes non-small cell lung cancer? Revised May 16, 2016. www.cancer.org/cancer/non-small-cell-lung-cancer/causes-risks-prevention/what-causes.html. Accessed May 26, 2019.
- Scholz N. Personalised medicine: the right treatment for the right person at the right time. European Parliamentary Research Service briefing. October 2015. www.europarl.europa.eu/RegData/etudes/BRIE/2015/569009/EPRS_BRI(2015)569009_EN.pdf. Accessed May 24, 2018.
- Silver J. Cancer prehabilitation: important lessons from a best practices model. The Oncology Nurse. 2015;8:1,8,9,14.
- Lungcancer.org. Lung cancer 101: your treatment team. Accessed May 24, 2018.
- Raez LE, Santos ES, Rolfo C, et al. Challenges in facing the lung cancer epidemic and treating advanced disease in Latin America. Clin Lung Cancer. 2017;18:e71-e79.
MAT-USO-NON-19-00060