Case: Sarah is a 28-year-old female who was recently diagnosed with early-stage breast cancer. Her oncology team has recommended that she receive TCHP (Taxotere + carboplatin + Herceptin + Perjeta) and have a mastectomy with reconstruction, followed by 5 years of tamoxifen. She was told that chemotherapy may impact her ability to have a child in the future. Sarah is recently engaged, and she and her fiancé strongly desire having biological children. Sarah’s oncologist refers her to a reproductive endocrinologist to discuss options for preserving fertility prior to starting treatment.
For premenopausal women like Sarah, treatments for breast cancer can pose a risk to their fertility—their ability to have biological children—in the future. With other things on your mind like finishing school, building your career, or finding a partner, you may not be thinking about having children before your cancer diagnosis. While fertility may not be on your radar, it is a topic that may be important to discuss with your oncologist at the time of diagnosis and treatment planning. Advances in reproductive medicine allow for patients to take steps to preserve their fertility in a timely fashion that is in line with their time frame for starting cancer treatments.
What Treatments for Breast Cancer May Impact My Fertility?
Not all cancer treatments impact fertility in the same way. Some treatments have minimal risk to fertility, while others are much more likely to have an impact. Chemotherapies classified as alkylating agents are associated with a higher risk to fertility than other types of chemotherapies. Oncologists and reproductive endocrinologists can help you determine what your personal risk to fertility may be based on your treatment plan and age.
Age is an important factor when determining your risk for infertility when beginning treatment for breast cancer. Women are born with all of the eggs they will ever have, and chemotherapy can significantly decrease that number of eggs. Generally, younger patients will have a higher ovarian reserve—a higher number of eggs—prior to starting treatment than older patients, so even if their egg count drops because of their treatment, it may not drop low enough to put them into menopause. Menopause is when the ovaries stop releasing eggs and menstrual periods stop. Patients may become menopausal earlier than they would have without cancer treatment, but they may still have many fertile years after completing treatments. An older but still premenopausal patient will have a naturally lower egg supply because of her age. When they begin chemotherapy, their egg count may drop to a level low enough to induce early menopause more quickly.
Many breast cancer treatment plans include 5 to 10 years of hormone therapy (eg, tamoxifen). It is generally not recommended to get pregnant while on these medications due to potential impacts to the unborn child. Although these drugs do not directly impact fertility, the length of time that a patient needs to delay having a child while on these medications may come with a natural, age-related decrease in fertility. Depending on age, many women consider fertility preservation prior to starting these medications.
What Options Exist to Preserve My Fertility?
Oncofertility is a term coined in 2007 to describe a field that joins oncology and reproductive medicine to improve patients’ options for biological parenthood through fertility preservation. In the field of oncofertility, there are a number of fertility preservation options that patients like Sarah might consider. These include embryo cryopreservation, oocyte cryopreservation (egg freezing), use of medications to help protect the ovaries, and ovarian tissue cryopreservation.1-3 It is important to speak with your medical team, including your oncologist and a reproductive specialist, about your potential interest in fertility preservation early, and ideally before beginning treatment, so that your options might be explored.
Embryo Cryopreservation
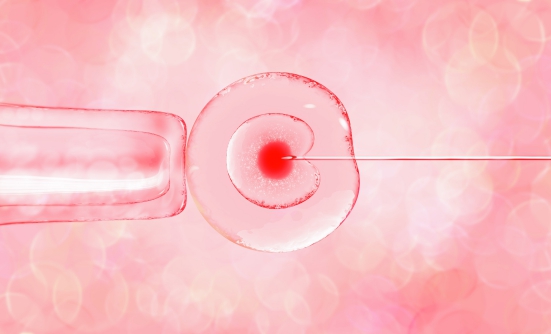
Embryo cryopreservation involves taking medications to cause the ovaries to release more eggs and then surgically retrieving mature eggs. Recent advances in reproductive medicine mean that patients do not have to wait for their menstrual cycle to begin the process of embryo cryopreservation. While this process previously took as long as 4 weeks, it now may take as little as 2 weeks. Next, mature eggs are fertilized in a lab with a male partner’s or donor’s sperm and cryopreserved (frozen) for later use thorough procedures like in vitro fertilization (IVF).
Oocyte Cryopreservation
Oocyte cryopreservation also involves taking medications to cause the ovaries to release more eggs, followed by surgical retrieval of mature eggs. As with embryo cryopreservation, this process may now be completed in as little as 2 weeks. Mature eggs are cryopreserved for later use through procedures like IVF.
Gonadotropin-Releasing Hormone (GnRH) Agonists
Medications called GnRH agonists (eg, goserelin, leuprolide) may also be recommended for use during treatment to help protect the ovaries. The goal with these medications is to reduce the chance that the ovaries stop working before they typically would (eg, premature ovarian insufficiency).
Ovarian Tissue Cryopreservation
A newer option, which may not yet be available at all sites, called ovarian tissue cryopreservation involves surgical removal of ovarian tissue and cryopreservation for later use. This procedure does not require any pretreatment medications and can be completed as soon as the procedure is scheduled, making it a useful procedure for patients who need to start treatment quickly. The cryopreserved ovarian tissue can be stored for many years and later re-implanted in the body to make pregnancy possible.
How Do I Find a Fertility Clinic?
While many large health systems have an affiliated fertility clinic, community cancer centers and other health systems may not. Talk with your oncologist to see if they have recommendations for, or have partnered with, a fertility clinic. The Alliance for Fertility Preservation and Livestrong have search functions on their websites, and the Oncofertility Consortium has a hotline (866-708-FERT) to help patients locate a fertility clinic in their area.
Who Can Help Me Think Through My Options?
Fertility preservation is a complex process with many decision points. On top of an already emotionally stressful time with navigating a recent cancer diagnosis, fertility-related decisions are further complicated by the emotional distress a patient may experience after learning that their cancer treatments may impact their ability to have biological children. Patients may experience feelings of grief or loss, rage, injustice, fear, sadness, frustration, shock, anger, worry, nervousness, uncertainty, and a loss of control over their ability to build their families.4 It is important for patients to feel like they are making an informed decision about fertility preservation, including whether to preserve or not. It may be helpful for you to connect with a multidisciplinary care team who can provide you with accurate fertility information and decision support and validate any fertility-related concerns you may have.
In addition to your cancer care team, your fertility care team may involve a reproductive endocrinologist, psychosocial provider, and/or an oncofertility navigator.
Reproductive Endocrinologist
Reproductive endocrinologists are fertility specialists. In conjunction with a patient’s oncologist, reproductive endocrinologists will review a patient’s treatment plan and provide them with a personalized estimate of their risk for infertility and their options for fertility preservation. If a patient chooses to preserve their fertility, reproductive endocrinologists will manage and conduct any fertility preservation–related medical procedures (eg, egg retrieval).
Psychosocial Providers
Psychosocial providers, like a mental health counselor, family therapist, social worker, or psychologist, can help patients process the emotions they are experiencing and assist with making a fertility preservation decision that best matches their goals and values.
Oncofertility Navigators
Some institutions may also have oncofertility navigators. These individuals provide fertility-related education and support and reduce barriers to preservation by coordinating fertility-related appointments and providing patients with information and resources.
Sarah and her fiancé are unsure about what steps to take after learning her fertility may be impacted by her breast cancer treatments. Sarah’s oncologist helped to connect her with an oncofertility navigator who got her scheduled for a consultation with a reproductive endocrinologist. Sarah and her fiancé also set up an appointment with a psychosocial provider, who helped them to evaluate their goals for family building and talk through Sarah’s fertility preservation options.
How Much Does Fertility Preservation Cost?
The cost for fertility preservation varies depending on procedure type. Costs can range from $11,000 to $15,000 for embryo cryopreservation, $10,000 to $15,000 for oocyte cryopreservation, and $500 to $1800 per injection for GnRH agonists (eg, leuprolide) without insurance.5 Patients may face additional costs associated with embryo or oocyte storage ($300-$600 per year) and to use preserved embryos or oocytes in the future through IVF or through the use of a gestational carrier (eg, surrogate).
As of June 2022, only 12 states have mandated insurance coverage of fertility preservation. It is important to contact your insurance provider to learn whether any portions of the fertility preservation process are covered. For many patients, fertility preservation is an out-of-pocket cost.
What Resources Exist to Help Me Pay for Fertility Preservation?
Some resources exist to help patients pay for fertility preservation. Livestrong Fertility partners with fertility clinics to provide discounted services and fertility medications to patients undergoing fertility services due to a cancer diagnosis. It is important to ask your fertility clinic if they have a partnership with Livestrong or a similar organization. There are other programs that can also help provide free fertility medications to patients with cancer undergoing fertility preservation. Heartbeat and ReUnite, offered by Ferring Pharmaceuticals and MDRx Fertility Pharmacy, respectively, are 2 examples.
There are also grants that patients can apply for to help decrease the cost of fertility preservation or storage. Verna’s Purse is a grant for people with cancer storing embryos or oocytes through ReproTech, a popular storage facility. Patients are eligible for discounted storage if they meet certain income criteria. Team Maggie’s Dream is a nonprofit organization that provides grants to people between the ages of 15 and 37 years pursuing fertility preservation ahead of cancer treatment. They award grants based on need and available funding, and awards can be used for embryo or oocyte cryopreservation, or a year of storage fees. The fertility clinic staff or oncofertility navigator may have access to additional resources to assist in paying for fertility preservation. When a patient is ready to use a preserved embryo or oocyte to build their family through IVF or the use of a gestational carrier, organizations like The Samfund have grants that patients can apply for to help cover some of the costs.
If I Do Not Preserve My Fertility, What Are My Options for Building a Family?
When a patient is not able to, or chooses not to, undergo fertility preservation, there are a number of potential options for family building after cancer treatment if this is important to them. Some patients will conceive naturally after breast cancer treatment, without medical intervention. If medical intervention is needed, there are a number of assisted reproductive technologies that may be useful. These may include IVF using a patient’s own oocytes and a partner or donor’s sperm, using donor oocytes or embryos and carrying the pregnancy themself, or using a gestational carrier. Adoption is another important option that may be the best fit for some families.
If you are interested in family building after treatment, it is important for you to bring this up with your medical team early, even if you are not yet ready to begin building your family. Your medical team may recommend a referral to a fertility specialist so that you may have an evaluation of your fertility. Bringing up potential interest in family building early will better help your medical team to connect you with information and support to make informed decisions.
References
- Shah NM, Scott DM, Kandagatla P, et al. Young women with breast cancer: fertility preservation options and management of pregnancy-associated breast cancer. Ann Surg Oncol. 2019;26:1214-1224.
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033.
- Ulrich ND, Raja NS, Moravek MB. A review of fertility preservation in patients with breast cancer. Best Pract Res Clin Obstet Gynaecol. 2022;82:60-68.
- Logan S, Perz J, Ussher JM, et al. Systematic review of fertility-related psychological distress in cancer patients: informing on an improved model of care. Psychooncology. 2019;28:22-30.
- Alliance for Fertility Preservation. Paying for Treatments. www.allianceforfertilitypreservation.org/paying-for-treatments/. Accessed July 1, 2022.
Resources
- Alliance for Fertility Preservation
www.allianceforfertilitypreservation.org/ - Oncofertility Consortium Fertline
https://oncofertility.msu.edu/
Financial Resources
- Livestrong Fertility Discount Program
www.livestrong.org/what-we-do/program/fertility - ReUnite Oncofertility
www.mdrusa.com/oncofertility/reunite-oncofertility/ - Heartbeat
www.ferringfertility.com/patient-resources/ - Team Maggie’s Dream
www.teammaggiesdream.org/ - Verna’s Purse
www.reprotech.com/vernas-purse/ - The Samfund
www.thesamfund.org/