LUNGevity and four other lung cancer organizations are issuing regular joint statements on coronavirus to help people understand what is known about the disease, find reliable sources of information, and be aware of its potential impact on vulnerable populations, including those with lung cancer.




March 16, 2020
Update to the Joint Statement on Coronavirus COVID-19 from Lung Cancer Advocacy Groups
Download the updated statement for the week of March 16, 2020.
The World Health Organization officially declared the COVID-19 outbreak a pandemic on March 11, 2020. As cases of the virus surge in countries around the world, with Italy being particularly hard hit, many nations are taking extreme steps to mitigate the outbreak, including whole country lockdowns. Here in the United States, the President declared a national emergency on March 13, 2020.
In this week’s update, we discuss four important topics related to COVID-19.
1. Social distancing and why it matters for COVID-19
COVID-19 is caused by the virus SARS-CoV-2. Individuals infected with SARS-CoV-2 appear to shed the virus from their respiratory tract (e.g., when coughing) even when symptoms may be very minor. Individuals infected with SARS-CoV-2 appear to shed the virus from their respiratory tract during the prodromal period.1 The prodromal period is part of an infectious disease cycle. It is defined as the period during which the symptoms felt by an infected individual may not be very specific or severe. The infected person can still perform usual functions and can therefore continue to be infectious. An infected individual can shed virus with very minor signs and symptoms.2 This explains why we are seeing widespread transmission in the community (this didn’t happen with SARS).
The reproductive number (R0) – the number of secondary infections generated from one infected individual – is estimated to be between 2 and 2.5 for COVID-19 virus.3 This means that a single infected person infects 2.5 people, which is higher than for the influenza virus. Approximately 3 to 5 days after infection, a person starts shedding virus and can infect others. Therefore, within a month, a single case can lead to 244 new cases.
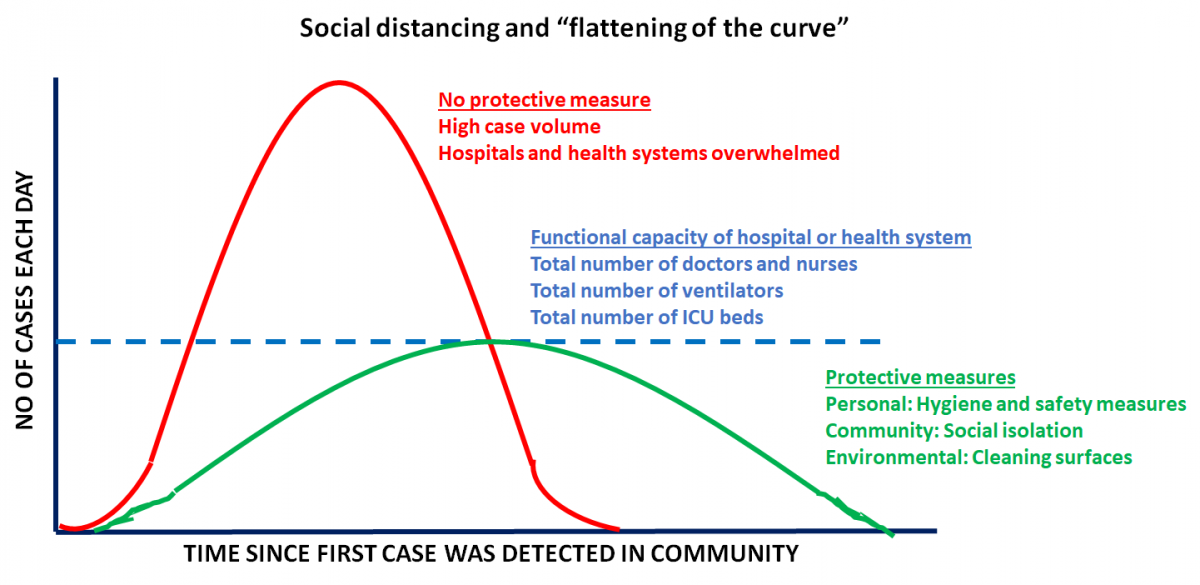
The CDC now recommends social distancing to help decrease transmission of COVID-19 within the community.4 Social distancing measures, such as cancelling public gatherings and avoiding crowds, can slow the spread of the virus and spread cases out over a longer period of time, which can help hospitals provide care while avoiding being overwhelmed by patients. Social distancing helps “flatten the curve” in the spread of an infectious disease. This is especially critical because hospitals and health systems are working at full capacity. Flattening the curve ensures that systems are functional and people who require care the most can get the attention they need. The CDC recommends a distance of 6 feet or 2 meters as the minimum distance between individuals.5
In case you are interested, we invite you to take a look at the CDC’s community transmission mitigation strategy document (cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf).
2. Appointments with your oncologist: virtual or in-person?
It may be a good idea to consider rescheduling or switching to a virtual appointment if your treating physician or cancer center provides this option. Note that virtual appointments are not appropriate for infusions for chemotherapy or immunotherapy, or potentially critical scans. If you have an oncology visit due in the next couple of months, please contact your treating physician as soon as possible to discuss what’s the right approach for you and whether they anticipate any drug shortages due to supply chain disruption.
Several hospitals are now limiting the number of visitors and/or people accompanying patients to no more than one at a time. In Seattle, the area hardest hit with cases, some hospitals are implementing the following measures to avoid being overwhelmed6:
- People with routine appointments are being screened for symptoms. Those who are sick are required to wear a mask or may not be allowed to enter the clinic.
- Elective surgeries are being postponed.
- Patients who have flu-like symptoms or other concerns are asked to CALL their doctor rather than going directly to the Emergency Department or Urgent Care.
- If you are having difficulty breathing, please do go to the Emergency Department.
3. COVID-19 testing: where we are now
We are seeing transmission in the community, so it’s likely the virus is more widespread in the United States than we imagine. However, we don’t have hard data because testing was not implemented in the earlier days of the epidemic in the US.7 Right now, most people need to have symptoms before they can be tested. As more test kits are distributed, testing will hopefully expand. Drive-through testing has been made available in a few locations but is not yet widely available. As we have stated previously, the symptoms of COVID-19 infection include fever, dry cough and shortness of breath. If you suspect that you have been infected, you should call your doctor or local health department to determine next steps. The availability of tests varies on where you live.
The CDC is maintaining an updated list of where tests are currently being performed in the US.8
Additionally, state health departments are a valuable resource, providing hotlines and websites with information about what to do if you are concerned that you or a loved one might be infected (links in the references).
4. Voices from the community
Please check out Janet Freeman-Daily’s article where she describes her experience as a lung cancer survivor with a cough and the difficulties she faced to get tested for COVID-19. Janet lives in the Seattle, WA area, a COVID-19 hotspot.
Fred Hutchinson Cancer Research Center in Seattle published a helpful blog post, “Coronavirus: what cancer patients need to know.”
Resources and websites:
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. Coronavirus: What People with Cancer Should Know - https://www.cancer.gov/contact/emergency-preparedness/coronavirus
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC), which can be found here:
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Johns Hopkins Coronavirus Resource Center is one of the best places to get current updates. https://coronavirus.jhu.edu/
- You can find information specific to your state or city or town on your health department’s website.
- A list of state department of health websites can be found here: https://www.cdc.gov/publichealthgateway/healthdirectories/healthdepartments.html
- A list of local health department websites can be found here: https://www.naccho.org/membership/lhd-directory
- The American Medical Association is also maintaining a resource website for healthcare providers. You can find more information here: https://www.ama-assn.org/delivering-care/public-health/covid-19-2019-novel-coronavirus-resource-center-physicians
- If you cannot avoid air travel, check out this handy article on “Dirtiest Places on Airplanes: How to Avoid Germs”: https://time.com/4877041/dirtiest-places-on-airplanes/
References
- Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
- Hoehl S, Berger A, Kortenbusch M, et al. Evidence of SARS-CoV-2 Infection in Returning Travelers from Wuhan, China. N Engl J Med. 2020.
- WHO. Coronavirus disease 2019 (COVID-19) Situation Report – 46. 2020.
- CDC. Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission Coronavirus Disease 2019 (COVID-19) Web site. cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf. Published 2020. Accessed March 15, 2020.
- CDC. IInterim US Guidance for Risk Assessment and Public Health Management of Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures: Geographic Risk and Contacts of Laboratory-confirmed Cases. Coronavirus Disease 2019 (COVID-19) Web site. https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html. Published 2020. Accessed March 15, 2020.
- UW. COVID-19 (formerly called Novel Coronavirus). https://www.uwmedicine.org/coronavirus. Published 2020. Accessed 2020, March 15.
- Lambert J, Saey TH. Social distancing, not travel bans, is crucial to limiting coronavirus’ spread. Science News2020.
- CDC. Testing in U.S. Coronavirus Disease 2019 (COVID-19) Web site. https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html. Published 2020. Accessed March 15, 2020.
March 9, 2020
Update to the Joint Statement on Coronavirus COVID-19 from Lung Cancer Advocacy Groups
Download the updated statement for the week of March 9, 2020.
As advocacy organizations dedicated to serving the needs of lung cancer patients, all of us are closely monitoring the latest developments related to the outbreak caused by the novel coronavirus, SARS-CoV-2, and the resulting disease, COVID-19.
In this update, we have included additional information on facts about COVID-19, symptoms, testing, information about populations at risk of serious infection, and what you should do to protect yourself from COVID-19.
We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC), which can be found here:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
https://www.cdc.gov/coronavirus/2019-ncov/index.html
Facts about SARS-CoV-2/COVID-19
- This novel virus presents a unique threat to vulnerable populations, including the elderly and those with weakened immune systems, including cancer patients. Early studies conducted on lung cancer patients undergoing surgery suggest that this virus readily infects the lungs and can potentially cause pneumonia, making lung cancer patients particularly susceptible.1
- Research suggests that the overall clinical consequences of COVID-19 may ultimately be similar to those of a severe seasonal influenza or a pandemic influenza.2
- SARS-CoV-2 is very infectious. Infected individuals may not show symptoms of COVID-19 but are still considered infectious.3
Symptoms of COVID-19
Symptoms may appear 2-14 days after exposure and may include:
- Fever
- Tiredness
- Dry cough
- Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually.
- Some people become infected but don’t develop any symptoms and don't feel unwell.
Can I get tested for COVID-19?
As of today, the CDC recommends testing symptomatic individuals. Clinicians should use their judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested.4
Who are at increased risk of developing a serious form of COVID-19?
- Recent data suggest that certain populations may be at higher risk of getting very sick from infection with SARS-CoV-2. These groups include:
- People with cancer.5 Though the numbers are very small (5 out of 18 patients included in the study), research suggests that lung cancer patients may be susceptible to a more serious form of the infection
- People with lung disease,6 such as COPD (chronic obstructive pulmonary disease)
- People with hypertension (high blood pressure)7
- People with diabetes7
- People with heart disease6
- People with kidney disease8
- Older adults, defined as those above the age of 606,8
- People in active cancer treatment or whose immune systems may be compromised by chemotherapy or steroids9
- If you have more than one of the risk factors described above, you may be at an even greater risk of developing a serious form of COVID-19.
What you can do:
- If you or a loved one are in one of the high-risk groups described above:
- Stay at home as much as possible.
- Make sure you have access to several weeks of medications and supplies in case you need to stay home for prolonged periods of time.
- When you go out in public, keep away from others who are sick, limit close contact and wash your hands often.
- Avoid crowds, especially in poorly ventilated spaces.
- Stay up to date on CDC Travel Health Notices (https://wwwnc.cdc.gov/travel/notices).
- Plan now for what you will do if you, or people you rely on for support, become ill
- We encourage everyone to follow best practices for public health, such as staying home when ill, handwashing with soap and water (or using a hand sanitizer), and respiratory etiquette including covering the mouth and nose during sneezing and coughing.10 Many of the steps you would take to protect yourself from catching the flu also apply for protecting yourself against COVID-19.
- Regarding travel within the United States, at this time the CDC is encouraging limited travel restricted only to essential travel. We encourage all people to evaluate the need for non-essential travel and to take appropriate precautions if travel is required. Please check with your doctor before making international travel plans. Again, the CDC is maintaining a page that outlines current travel advisories: https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html
What you should not do:
Do not read or share information about COVID-19 from websites that are not maintained by reputable public health organizations (for example, the CDC). When in doubt, check your facts with what’s posted on the CDC or WHO website.
Treatment and Vaccines:
- As of now, there are no treatments for COVID-19. All treatments involve simply reducing the symptoms of the infection.
- As of now, there are no vaccines to prevent a COVID-19 infection.
Resources and websites:
- You can find information specific to your state or city or town on your health department’s website.
- A list of state department of health websites can be found here: https://www.cdc.gov/publichealthgateway/healthdirectories/healthdepartments.html
- A list of local health department websites can be found here: https://www.naccho.org/membership/lhd-directory
- The American Medical Association is also maintaining a resource website for healthcare providers. You can find more information here: https://www.ama-assn.org/delivering-care/public-health/covid-19-2019-novel-coronavirus-resource-center-physicians
- If you cannot avoid air travel, check out this handy article on “Dirtiest Places on Airplanes: How to Avoid Germs”: https://time.com/4877041/dirtiest-places-on-airplanes/
References:
- Tian S, Hu W, Niu L, Liu H, Xu H, S. X. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. Journal of Thoracic Oncology. 2020.
- Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the Uncharted. N Engl J Med. 2020.
- Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020.
- CDC. Evaluating and Reporting Persons Under Investigation (PUI) Summary of Recent Changes. Coronavirus Disease 2019 (COVID-19) Web site. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html. Published 2020. Accessed March 8, 2020.
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335-337.
- CDC. People at Risk for Serious Illness from COVID-19. Coronavirus Disease 2019 (COVID-19) Web site. https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html. Published 2020. Accessed March 8, 2020.
- Guan W, Lian W, COVID-19 on behalf of China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1,590 patients with COVID-19 in China: A Nationwide Analysis. medRxiv. 2020.
- Liu Y, Sun W, Li J, et al. Clinical features and progression of acute respiratory distress syndrome in 2 coronavirus disease 2019 medRxiv. 2020.
- Center FHCR. Coronavirus: what cancer patients need to know. https://www.fredhutch.org/en/news/center-news/2020/03/coronavirus-what-cancer-patients-need-to-know.html. Published 2020. Accessed March 8, 2020.
- Del Rio C, Malani PN. 2019 Novel Coronavirus-Important Information for Clinicians. JAMA. 2020.
March 3, 2020
Joint Statement on Coronavirus COVID-19 from Lung Cancer Advocacy Groups
We understand and appreciate the severity of the new coronavirus epidemic (also known as COVID-19) that’s spreading globally. As advocacy organizations dedicated to serving the needs of lung cancer patients, all of us are closely monitoring the latest developments related to the outbreak caused by the novel coronavirus, SARS-CoV-2, and the resulting disease, COVID-19.
This is a rapidly evolving situation and we are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC), which can be found here:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen https://www.cdc.gov/coronavirus/2019-ncov/index.html
Facts about SARS-Cov-2/COVID-19
- This novel virus presents a unique threat to vulnerable populations, including the elderly and those with weakened immune systems, including cancer patients. Early studies conducted on lung cancer patients undergoing surgery suggest that this virus readily infects the lungs and can potentially cause pneumonia, making lung cancer patients particularly susceptible.1
- Research suggests that the overall clinical consequences of COVID-19 may ultimately be similar to those of a severe seasonal influenza or a pandemic influenza.2
What you can do
- First and foremost, we encourage everyone to follow best practices for public health, such as staying home when ill, handwashing with soap and water (or using a hand sanitizer), and respiratory etiquette including covering the mouth and nose during sneezing and coughing. Many of the steps you would take to protect yourself from catching the flu also apply for protecting yourself against COVID-19.
- Regarding travel within the United States, at this time there are no restrictions on travel. However, the situation may change rapidly. We encourage all people to evaluate the need for non-essential travel and to take appropriate precautions if travel is required. Please check with your doctor before making international travel plans. Again, the CDC is maintaining a page that outlines current travel advisories: https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html
What you should not do
Do not read or share information about COVID-19 from websites that are not maintained by reputed public health organizations (for example, the CDC). When in doubt, check your facts with what’s posted on the CDC or WHO website.
Resources and websites
- You can find information specific to your state or city or town on your health department’s website.
- A list of state department of health websites can be found here: https://www.cdc.gov/publichealthgateway/healthdirectories/healthdepartments.html
- A list of local health department websites can be found here: https://www.naccho.org/membership/lhd-directory
- The American Medical Association is also maintaining a resource website for healthcare providers. You can find more information here: https://www.ama-assn.org/delivering-care/public-health/covid-19-2019-novel-coronavirus-resource-center-physicians
- If you cannot avoid air travel, check out this handy article on “Dirtiest Places on Airplanes: How to Avoid Germs” https://time.com/4877041/dirtiest-places-on-airplanes/
References
- Tian S, Hu W, Niu L, Liu H, Xu H, S. X. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. Journal of Thoracic Oncology. 2020.
- Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the Uncharted. N Engl J Med. 2020. 3. Del Rio C, Malani PN. 2019 Novel Coronavirus-Important Information for Clinicians. JAMA. 2020.
This article was previously published on Lungevity.org.