I am a 29-year survivor of multiple myeloma, a deadly blood cancer for which there is no cure yet. When I was first diagnosed in 1992, the average survival of people with this cancer was about 3 years, but is currently about 7 years thanks to the approval of several novel, groundbreaking drugs. I participated in early clinical trials that helped 2 of the most widely used multiple myeloma drugs gain FDA approval.
In my first decade with this cancer, I had 3 stem-cell bone marrow transplants before being told that there was no other treatment that could keep me alive, and I should go to a hospice.
Clinical Trial
Instead of going to a hospice, my wife Kathleen and I relocated from Ohio to Boston, and in 2002 I joined a clinical trial at Dana-Farber Cancer Institute for an experimental drug that was only available in clinical trials. This saved my life and led to the FDA approval of the drug Velcade in 2003, which was a major breakthrough in the treatment of multiple myeloma.
Likely because of the full-body radiation and melphalan I had received, in 2013 I was diagnosed with treatment-related leukemia, so I had a fourth transplant, and I have been in remission since then.
I strongly believe that I am alive today primarily thanks to my Kathleen’s caregiving, along with compassionate support from family and friends. Excellent medical teams and persistence have also been critical.
Key Questions
Several key approaches and techniques help me and Kathleen deal with multiple myeloma and its physical and emotional effects on both of us.
I was only 42 when an oncologist diagnosed me with the most advanced stage of multiple myeloma. I had advanced lytic lesions (bone damage) in my skull, which can occur in multiple myeloma, as well as broken ribs and other bone damage.
Our approach of asking questions quickly helped. When diagnosed, I asked “How long do you believe I will live?” The oncologist did not want to answer, but I persisted until he said, “If you do nothing, you will live a few months, but if you do all you can, maybe 3 years, if all goes well.”
I managed to ask, “If you were in my shoes, what would you do?” The doctor paused, then said, “I would consider retiring and doing my bucket list while I still could.” I managed one last question: “If you were me, what doctor would you have treat your case? And don’t limit your choices to our hometown.”
This question seemed to surprise him, and he finally responded, “Case Western Reserve Medical School has an excellent hematologist oncologist who practices at Cleveland’s other major cancer center, University Hospitals of Cleveland. He sees more myeloma cases than I do.” We followed his advice.
Strength Through Support
I considered retiring and doing a bucket list, but then I remembered that a terrible sports injury I had back in the day had recovered over time. Recovery was long and hard, though, and my family’s support was key. Kathleen and I drew on this experience and decided to give multiple myeloma our best shot.
I am blessed to have Kathleen’s love, understanding, and tolerance. She gives me strength when most needed. Our strategy is for her to manage her own fitness, research multiple myeloma developments, and manage medications and difficult insurance discussions. I manage my health and follow my doctor’s orders.
I exercise daily in some form, believing that it makes me stronger to withstand the damage from chemotherapy. I document the results of my doctor visits and tests, and we both watch our diets.
I kept a paper pad of cancer notes in chronological order; capturing key information from appointments or tests helped me form questions for follow-up meetings. I plotted monoclonal protein and other key results to show trends, since my oncologist advised that trends were more important than a single test result. Knowing my “scorecard” is important.
We adopted the approach of only making one change to treatments at a time, to see the result of that change accurately.
My Medical Team
Early on, we tried to form partnerships with our medical team. For example, Kathleen found an Italian article discussing bone thinning, such as mine from multiple myeloma. Italian doctors found that giving monthly 2-hour treatments of bisphosphonate intravenously helped to prevent further bone damage. Kathleen reviewed her findings with my doctor and asked if this might help me.
The doctor read the article and told us that although he did not think this was used in the United States, he believed it was reasonable. So I began the bone-strengthening infusions in 1994. We were not aware of any American patient with multiple myeloma who used these drugs at the time.
We waited to share the cancer diagnosis with our sons in college, our siblings, parents, and friends until we knew the specifics. We found that it helped to inform more people to support us, and it allowed us to let go of some of our feelings. When we had to miss other commitments, other people stepped in to help.
An early decision was to do an autologous stem-cell transplant rather than wait to see how long the first remission, achieved through chemotherapy, would last. After the transplant, all I could do at first was make myself sit up in bed. Next, I made myself stand next to the bed for as long as possible. When feeling strong enough, I pulled the IV pole and pumps around the transplant floor, much to the nurses’ dismay.
I think of my daily exercise strategy as being able to “Sit, Stand, Walk, or Move,” depending on what I can safely push myself to do. A relative describes this approach as “On your feet, not your seat.”
Within a month of the first transplant, I was back serving clients and feeling good, but Kathleen was not herself. She was stressed, having nothing more to do for my cancer, except worry about when it would return.
A Pink Buick
That all changed after I drove to work one day and called her an hour later to say I was fine, but a pink Buick ran a red light and crashed into the driver’s side of my car. Kathleen was very upset and screamed, “How could you get in a car accident after all we’ve been through?”
She paused, and then realized it could happen to anyone. She tells people this helped ease her worry about cancer. None of us knows when our days will be over, cancer or not. And, she likes to add, “Watch out for those pink Buicks.”
My multiple myeloma eventually returned, and I pressed to do a second transplant, but the local doctor did not approve. He thought it was unlikely that enough stem cells could be harvested for a second transplant.
Second Opinion
This led to another key strategy we use: seeking a second opinion. We traveled to the Mayo Clinic in Rochester, Minnesota, where it was concluded that a second transplant was reasonable, so I had it done in Cleveland. We returned for another second opinion before my third transplant, and learned about a clinical trial of an experimental drug that showed good results for patients with advanced multiple myeloma.
This was life-saving, because the third transplant was not strong enough to control my myeloma cells, so as noted earlier, in 2002 I was advised by my local doctor to go to a hospice. Instead, I followed the Mayo Clinic’s advice to join a clinical trial.
Paul Richardson, MD, a multiple myeloma expert at Dana-Farber Cancer Institute was the doctor who returned my call and advised us to relocate to Boston for the clinical trial, which we did. I was very sick from the high level of myeloma cells: my legs were swelling, my temperature was 104, and I could not eat.
Within 2 weeks of receiving the experimental drug, 99% of the myeloma cells were in remission. We were told that no one at Dana-Farber had seen such dramatic results, which resulted in the FDA approval of Velcade. To us it was a miracle.
American Cancer Society
We discussed our good fortune of having resources that allowed us to relocate from Cleveland. Kathleen reminded me, “This is why the American Cancer Society (ACS) operates over 30 Hope Lodges around the country, where patients and caregivers needing to leave their hometown can get free lodging.” Kathleen began as a door-to-door volunteer fundraiser, and advanced to the ACS Board of Directors, receiving many volunteer awards.
While in Boston, Kathleen had an idea for raising awareness and funds for ACS Hope Lodges. I listened as she excitedly explained she could create a 4-day, 300-mile cycling event in Ohio, in which people would ride from Cleveland to Cincinnati, where each city had ACS Hope Lodges. Riders would raise money in support of their ride. It would be a bike tour on bike paths and country roads. College dorms could house riders and support ACS staff and volunteers.
I said, “Honey, that’s a good idea, except neither of us cycles, or even owns a bike.” She replied, “Not a problem; I will work with ACS management and staff and work that out.”
We have since also learned that the ACS funded the scientist whose research led the start-up drug company that developed Velcade.
Kathleen’s Volunteering
ACS leaders knew and respected Kathleen from her years volunteering on other projects, including her fundraising leadership for the Cleveland Hope Lodge, where she formed and led a volunteer Advisory Board.
I watched as she threw herself into overcoming challenges that her bike ride presented, especially because she had no cycling experience. The ACS leadership introduced her to Dennis, a volunteer who was an experienced cyclist. His cycling enthusiasm was matched with her passionate fundraising.
The Pan Ohio Hope Ride (www.POHR.org) became a 4-day, 328-mile bike tour, with riders staying in college dorms along the way. Kathleen visited a AAA office and studied country roads and bike paths between Cleveland and Cincinnati.
For 2 years, I watched Kathleen passionately turn her bike ride idea into a reality. I had to do more to support her hard work, so I consulted with Dennis, bought a road bike, and trained.
Before the first ride, a reporter asked our younger son, Bob, if he thought I could complete the long ride. Bob said, “I don’t know if Dad will do all the miles, but when Dad says he’ll do something, he’ll do it.” I remain touched by those words. Under the watch of our older son, Jim, and Bob’s wife, Stacey, I cycled the entire 328 miles in 4 days, and have done so for 12 years.
My cycling 328 miles in the ACS POHR changed my transplant doctors’ opinion on whether I could survive my fourth stem-cell transplant. The ACS is key to our survival story.
Sharing Our Story
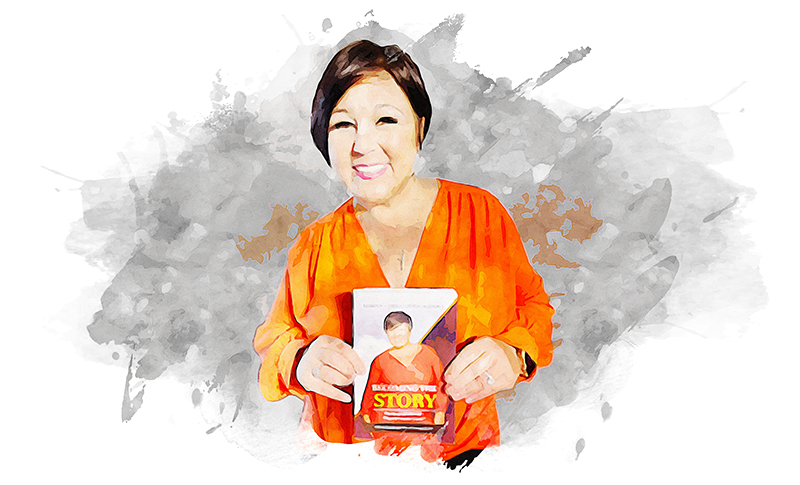
We shared our survival story hundreds of times with support groups in 40 states of the United States, and in Japan and Spain. Sharing our story helps us, and, we hope, helps other patients and caregivers. Support groups can contact me at
Since our self-imposed travel restrictions of COVID-19, we began sharing our story virtually with support groups, in podcasts, webcasts, and other venues. We virtually shared our story in Canada, New Zealand, and Latin America. Also during our lockdown, I wrote a book, The Man in the Arena: Surviving Multiple Myeloma Since 1992, which is now available at Amazon and at local bookstores. The profits go to charities. Our strategies and approaches are the book’s focus.