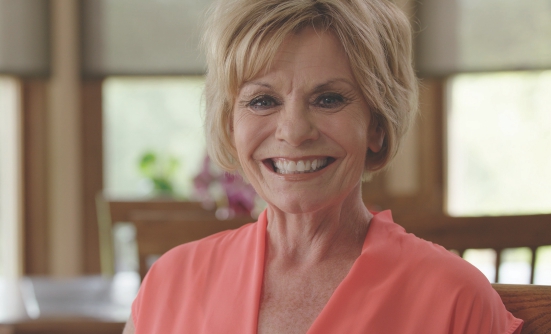
When you reach a certain age, aches and pains often become common. That’s why, as a woman in her mid-50s, I didn’t think much of it when I woke up one day with a backache. I figured that I had overexerted myself in some way, maybe by picking up one of my grandchildren or carrying something too heavy.
Lingering Back Pain
But when the pain lingered for longer than I thought would be considered acceptable, and even increased, I decided to visit my doctor, who suggested different treatments that are normally used to relieve back pain.
First came acupuncture, which did not help my pain. Next was a technique called muscle scraping, in which a tool was used to “scrape” back and forth over the muscles on my back to promote blood flow to that area, but just like acupuncture, it did nothing to relieve the pain.
Then a visit to a chiropractor, which was followed soon after to a physical therapist, both of whom said they couldn’t do anything to help me.
After a nearly 4-month journey of being poked and prodded, and frankly getting nowhere, my doctor finally agreed to send me for an MRI, in the hope that it would identify what was causing the pain.
I found it odd that none of the treatments or therapies I tried helped even a little, so when the doctor mentioned an MRI, I assumed that the cause could be more serious, such as a herniated disc or a pinched nerve.
It turns out I was right, and it was, indeed, serious, but not what I had thought. Imagine my surprise when the doctor sat me down and told me that I had cancer.
MRI Shows Metastatic Cancer
The MRI showed abnormal cells growing in several places in my body, which indicated I had cancer, but we still needed to find the primary site, where it began. After additional testing and biopsies, it was determined that the cancer started in my lungs, and then spread to my brain, lymph nodes, liver, and bones, which was causing my back pain.
With a diagnosis of stage IV lung cancer, meaning metastatic lung cancer that has spread to other parts of the body, the doctors gave me a prognosis of between 2 and 8 years to live.
My husband, children, and I had several crying sessions, but during one of these sessions, my husband reminded us that there was still hope.
“We’re going to live each day the best that we can. That’s what we’re going to do,” he said.
Molecular Profiling
As I waited to start my first round of chemotherapy, my daughter-in-law took my medical records and sent them to the Mayo Clinic in Rochester, Minnesota, to get a second opinion. When they got back to her, they asked if I had a molecular profile done to look for any biomarker that may be associated with my tumor.
I have to admit, I had no clue what a molecular profile was, let alone if I had one done. My oncologist, Tim Dorius, MD, explained that molecular profiling, also called genomic profiling or biomarker testing, is a test to see the genetic makeup of a tumor, which may help to determine how the cancer may progress, or which treatment may be the most beneficial for that specific tumor type.
Molecular profiling is done to see if the tumor is associated with a specific biomarker. Today, new targeted therapies and immunotherapies are being developed specifically to target certain biomarkers linked to some types of cancer, and these therapies have a greater chance of success than older therapies.
Dr. Dorius said that he had ordered this test for me from Caris Life Sciences that uses a tumor profiling approach called next-generation sequencing, and we were waiting for the results of the test. When the molecular profile report came in, Dr. Dorius told me that he had good news.
He said that my tumor had very high levels of a protein called PD-L1, a biomarker seen in some types of cancer. In fact, he said I had the highest level that he’d ever seen in a patient.
Targeting PD-L1 with Immunotherapy
This meant that I would not receive treatment with chemotherapy, but an immunotherapy that specifically targets PD-L1, the biomarker that is associated with my lung cancer. Dr. Dorius explained that certain immunotherapies today target PD-L1 in the tumor to boost the body’s immune response.
Many people who are told that they have cancer immediately think of chemotherapy and losing all their hair, as well as being sick and miserable from the side effects of chemotherapy. So I was shocked to learn that I would not have to go down that path, because immunotherapy does not have many of the side effects associated with chemotherapy. I was therefore grateful for the option to start treatment with immunotherapy.
A few months after starting immunotherapy, I woke up and had realized that the back pain that had plagued me for months despite the different treatments, was gone. My body was responding well to the treatment, probably because of the high levels of the PD-L1 biomarker in my tumor.
Never Lose Hope
Since starting treatment with the immunotherapy, the cancer that was in my bones, liver, and lymph nodes is gone entirely; in my brain, only dead scar tissue is left after I had radiosurgery. There is still a small spot remaining in my right lung, which my doctors continue to monitor carefully.
I now have my life back. We go on vacations. I watch my grandkids. I work outside. I go to work every day.
I continue to have full body scans every few months to make sure that the cancer has not come back or has not started to grow again. Each time, I am convinced that I’ll learn that the cancer had spread again.
I know that my body may not continue to respond to the immunotherapy in this positive way forever, but when and if or when that time comes, I do have the option to start treatment with chemotherapy.
Right now, I am just happy to have the option to be living my life the way I want, with such minimal side effects.
I always think back to my husband telling me to never lose hope, at a time when it looked as if I had very little hope left.
I now know that you never really know what the future holds. You could be that one person for whom a miracle is going to happen, or that one person who is going to be a survivor, despite the odds. I believe that this is going to be me.