The mysterious miracles of the human immune system are awe-inspiring; ebbing and flowing through the intricacy of harmonizing and negotiating “self” from “non-self.” Repulsed by intruders seeking to cause chaos, the immune system tirelessly searches the body. Every day it challenges foreign invaders, ridding them from the body and resetting its perfect balance. Bacteria and viruses enter as obvious intruders, unable to lie in wait. The immune system immediately conjures natural killer cells to unleash toxins to help eliminate or contain the bacteria or viruses so they can no longer reproduce (referred to as innate immunity).
The ultimate challenger, the cancer cell, mocks such tyranny. Cloaked in disguise, cancer cells roam freely, unrecognized and unwitnessed. Due to the cells’ likeness of self, the immune system quickly evades the kill, leaving cancer cells to secretly multiply and take refuge at free will.
But if the immune system is in full function, why and how does such invasion happen? This deceit from identity recognition happens when the surface of the cancer cell expresses proteins that inactivate an immune cell or through expression of tumor markers (antigens) on its surface causing further confusion. Baffled, the immune system foregoes its natural instinct to kill and remove the intruder. Based on the scientific principles that cancer cells can be identified as foe as opposed to friend, immunotherapy has entered the realms of cancer therapy; becoming the fourth pillar in cancer treatment.
The Role of Immunotherapy in Cancer Care
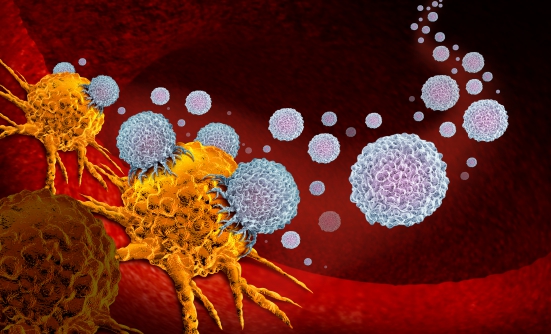
Immunotherapy has an uncanny, yet unobtrusive, ability to awaken the sleeping dragon—the immune system. By tapping into the unique powers of the immune system, immunotherapy provokes the body’s natural defenses to seek and destroy cancer cells. As if to conjure prowess, immunotherapy either marks cancer cells for destruction or bolsters the immune system to work vigorously against them. Thus, an awakened immune system is better equipped to hunt for cancer cells, stopping or slowing growth of the cancer, as well as its spread to other parts of the body.1-3
Types of Immunotherapy
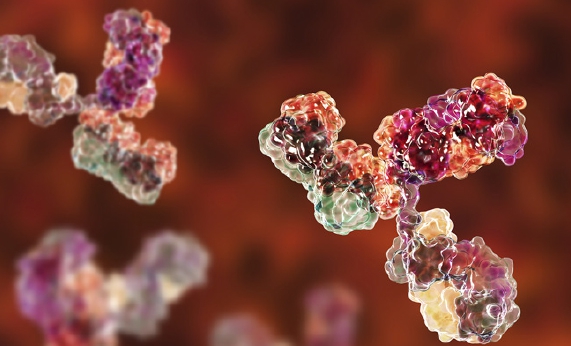
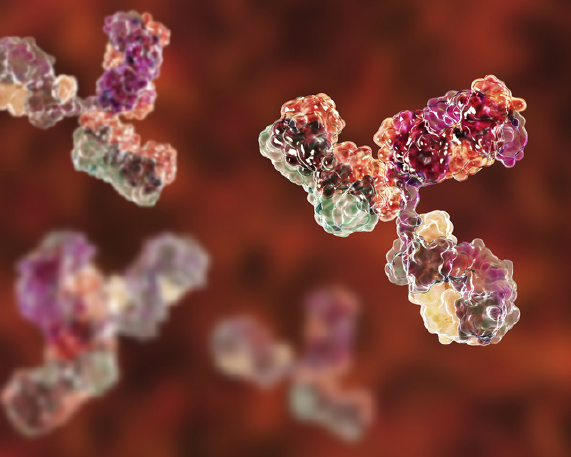
There are several forms of immunotherapy, including monoclonal antibodies, cancer vaccines, cytokines, adoptive cell transfer, and checkpoint inhibitors. Monoclonal antibodies are proteins used by the immune system to identify and target specific antigens found on the cancer cell. These antibodies (ie, bevacizumab, rituximab, trastuzumab) are responsible for cell death, obstruction of cell growth, or interference with cell function. Vaccines are used in cancer care either to aid in the prevention of cancer, like the human papillomavirus vaccine (Gardasil), or to treat cancer. Therapeutic vaccines are designed to teach immune cells to develop a deep memory so it can respond to specific cancer antigens.1 Sipuleucel-T (Provenge) is one example of an FDA-approved therapeutic vaccine for men living with advanced prostate cancer.4 Cytokines are a group of naturally produced signaling proteins that act like messengers to help control the growth and activity of immune system cells. Although not as readily available, nor used in a wide variety of cancers, adoptive T-cell therapy is another form of immunotherapy. Adoptive T-cell therapy is a multistep process of removing the T-cells from the patient, sending them to a specialized lab for modification, and then infusing them back into the individual so the modified T-cells can search and destroy the cancer cells.5
The most notable form of immunotherapy is immune checkpoint inhibitors. The immune system operates efficiently because of safeguards—checks and balances per se. These checkpoints act like “brakes” and are in place to keep the immune system from going into overdrive and destroying normal cells and tissue. When there is interruption of the checkpoints, the immune system views normal cells as “non-self,” resulting in autoimmune diseases. Cancer cells have the ability to overtake these same checkpoints, masking themselves from detection, and manipulating the body’s natural defensive response so they can continue to multiply. Checkpoint inhibitors remove the “brakes” so the immune system is able to unmask the cancer cells, attack, and kill them.1,6-8
Not All Are Created Equal
It must be noted that immunotherapy is not for everyone diagnosed with cancer. Although results may be impressive and long-lasting, statistically, only 1 in 5 will respond to immunotherapy. Many would ask, “Am I appropriate for immunotherapy?” Such a great inquiry, but a question only a medical oncologist can truly answer. Several factors come into play when determining if someone is appropriate to receive immunotherapy. It is not standard of care, as first-line treatment, for all cancer types nor all stages of the cancer. Those with autoimmune diseases, such as Crohn’s disease, multiple sclerosis, rheumatoid arthritis, and lupus, or who have undergone an organ transplant, may not be appropriate for immunotherapy due to the inflammatory response caused by the activation of the T-cells. If the cancer has taken a toll, and therapy needs to start quickly to control symptoms, chemotherapy may be the best first option due to the length of time it may take the immune system to recognize and attack the cancer cells. Clinical trial options abound as scientists defy the mystery of the immune system, unlocking its fullest potential in the treatment, and possible eradication, of cancer.
Understanding Self
It is true. The side effects may be gentler to the body than those experienced from chemotherapy, but do not confuse kinder and gentler with void of risks and toxicities. Although the most common side effects (fatigue, nausea, and musculoskeletal discomfort) can be mild and manageable, there are side effects requiring early recognition and reporting.9 Side effects to immunotherapy (often referred to as immune-related adverse effects) are not predicable. They may arise at any time throughout the treatment plan and up to a year after completion of therapy. It is important to remember that these side effects are the result of the immune system being overstimulated to the point it cannot recognize “self” as friend, erroneously attacking healthy tissue and cells. For this reason, it is imperative to report any and all symptoms and side effects to the healthcare team, no matter how insignificant they may seem. Personal awareness is key to early detection and early treatment. How many hours a day do you normally sleep? If you nap, how often and how long? Examine your skin. Do you have any rashes or skin changes prior to starting immunotherapy? How far can you walk before you need to stop to catch your breath? If you have a cough, what aggravates it? Does it happen every day? Are you able to complete your daily hygiene activities without rest periods? How frequently do you have a bowel movement? Is it daily? Is it 4 times a week? Personal questions, yes. Necessary to answer, absolutely. Rationale, could be life-saving.6,10,11
Conclusion
Although not appropriate for all diagnosed with cancer, immunotherapy has changed the platform of cancer care. Whether given alone, with chemotherapy, or after chemotherapy and radiation, immunotherapy has the potential to improve survival in those undergoing cancer treatments. It is propelling cancer into a chronic disease. As puzzling as the human immune system is, does it not elicit fascination and bewilderment for what the future of medicine will bring?
Patient Resources
American Cancer Societywww.cancer.org
Cancer Support Community
https://cancersupportcommunity.org
National Cancer Institute
www.cancer.gov
Society for Immunotherapy of Cancer
www.sitcancer.org/home
References
- Makkouk A, Weiner GJ. Cancer immunotherapy and breaking immune tolerance: new approaches to an old challenge. Cancer Res. 2015;75:5-10.
- Yang Y. Cancer immunotherapy: harnessing the immune system to battle cancer. J Clin Invest. 2015;125:3335-3337.
- Bindea G, Mlecnik B, Angell HK, Galon J. The immune landscape of human tumors: implications for cancer immunotherapy. Oncoimmunology. 2014;3:e27456.
- Cheever MA, Higano CS. Provenge (Sipuleucel-T) in prostate cancer: the first FDA-approved therapeutic cancer vaccine. Clin Cancer Res. 2011;17:3520-3526.
- Kalos M, June CH. Adoptive T cell transfer for cancer immunotherapy in the era of synthetic biology. Immunity, 2013;39:49-60.
- Hedge PS, Karanikas V, Evers S. The where, the when, and the how of immune monitoring for cancer immunotherapies in the era of checkpoint inhibitors. Clin Cancer Res. 2016;22:1865-1874.
- Rubin KM. Understanding immune checkpoint inhibitors for effective patient care. Clin J Oncol Nurs. 2015;19:709-717.
- Brahmer JR, Pardoll DM. Immune checkpoint inhibitors: making immunotherapy a reality for the treatment of lung cancer. Cancer Immunol Res. 2013;1:85-91.
- Howell M, Lee R, Bowyer S, et al. Optimal management of immune-related toxicities associated with checkpoint inhibitors in lung cancer. Lung Cancer. 2015;88:117-123.
- Cousin S, Seneschal J, Italiano A. Toxicity profiles of immunotherapy. Pharmacol Ther. 2018;181:91-100.
- Haanan JB, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment, and follow-up. Ann Oncol. 2017;28(suppl 4):iv119-iv142.