One health consideration for all women is when to begin breast cancer screening. The gold standard test for breast cancer is the mammogram. For the uninitiated, mammograms are essentially an x-ray of the breasts taken from different angles and can locate tumors that are not discovered during breast exams.
When is the proper age to get the test? That depends on a couple of different factors. To start, mammogram guidelines differ, which can leave women uncertain about when they should get screened. The US Preventive Services Task Force mammogram guidelines recommend women begin screening at age 50, the American Cancer Society recommends women begin screening at age 45, and the National Comprehensive Cancer Network and American College of Radiology recommend women begin screening at age 40.
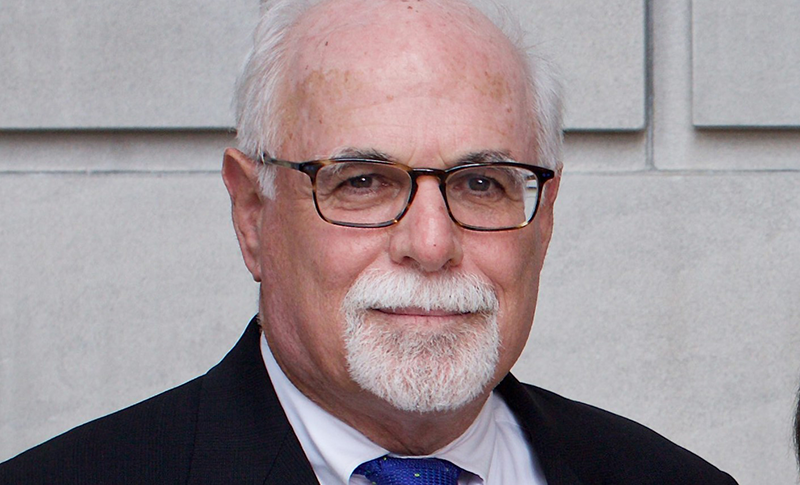
Deborah Rhodes, MD, Mayo Clinic, says it’s important to remember these are general guidelines. “The reason that the guidelines differ so much is that there is no perfect answer about when women should start,” explains Rhodes. “These guidelines are for average-risk women. It is really important for each woman to work with her healthcare provider to discuss her risk factors for breast cancer and her screening preferences in order to develop an individualized approach to screening. All of the screening and prevention interventions depend upon an accurate understanding of your breast cancer risk and your goals.”
Rhodes is an internal medicine specialist who practices at Mayo’s Breast Clinic, and says women need to know their own family medical histories along with understanding the nuances of mammograms’ diagnostic capabilities to help in the decision-making process.
For Women with an Average Risk for Breast Cancer
Rhodes says there is controversy regarding when women at average risk for breast cancer should begin screening and how often screening should be done. Although no approach is universally accepted, some factors should be considered when weighing mammography testing on an annual or every-other-year basis for women under the age of 50, explains Rhodes.
“It really takes an understanding of the risk/benefit ratio. The risk is, you might be called back for additional testing that, in retrospect, was not necessary. The benefit is, you can find the cancer earlier so that it could be cured. Women need to look at that risk/benefit ratio and how likely they are to have a cancer detected and how unlikely they are to undergo an unnecessary procedure. Based upon those factors, they need to decide for themselves whether they want to go through this every year or every other year.”
For women in their 40s, one important nuance of the test is that mammograms sometimes do not identify tumors, or conversely, the test picks up things that require further testing. This latter result can involve invasive procedures such as biopsies, cause undue stress, and end up being a false-positive result.
Rhodes points out that women in their 40s may have denser breast tissue, and therein lies the challenge.
“The more dense the tissue in the breast, the harder it is to distinguish the tumor from that dense tissue, because both tumors and dense tissue look white on a mammogram,” says Rhodes. “It’s not that the radiologist missed it, because that is rare, but a tumor might be surrounded by the dense tissue and therefore not visible. Mammography is very effective in women who don’t have dense breast tissue, but we need to individualize screening guidelines for women with dense tissue and offer more effective testing. The approach now is that women can choose to have mammography plus another test.”
Other Screening Tests
Although mammograms remain the gold standard for breast cancer screening, other supplemental screening tests are available. Rhodes provided a brief overview on the effectiveness and challenges of these tests.
- Standard MRI
Rhodes points out that this test is more sensitive than a standard mammogram. The challenge is that MRIs are very expensive and cost-prohibitive to run annually. In addition, some women’s medical conditions preclude them from it, and some patients have claustrophobia and cannot undergo the test. Due to these factors, MRI screening is currently limited to women at high risk for breast cancer. - Abbreviated form of MRI
This test is not as lengthy, so it is less expensive. This test is currently being studied to determine if it is more effective than 3D mammography in finding tumors in dense breasts. - Contrast-enhanced mammography
This mammogram is used in conjunction with an iodine dye injection that can highlight a tumor in a bed of dense tissue. The challenge of this test is that some people are allergic to iodine dye. - Whole breast screening ultrasound
In some centers, this is being offered in addition to mammography for women with dense tissue. The challenge, explains Rhodes, “is that it tends to lead to a lot of unnecessary biopsies in order to find very few additional tumors.” - Molecular breast imaging
“This is a relatively new test that is about 3 to 4 times more effective in identifying cancers than mammograms in women with dense tissue,” says Rhodes. “This is a different way of imaging the breast tissue using a tracer that is absorbed by the tumor but not by the background dense tissue,” says Rhodes.
For Women with a Higher Risk for Breast Cancer
Rhodes indicates that the average-risk guidelines for breast cancer screening do not apply to women with risk factors such as a family history of breast cancer. In general, women who have a family history of breast cancer should have an annual mammogram starting no later than 10 years before the age of the earliest diagnosis in the family (but not earlier than age 25 and not later than age 40). Women who have inherited a breast cancer gene mutation or have a family history suggestive of a possible breast cancer gene mutation are advised to begin screening as early as age 25.
She believes all women who have a family history of breast cancer should have a breast cancer risk assessment and discuss with their provider when they should start screening, as well as whether they should consider additional screening tests beyond a mammogram and preventive options.
For women with a higher risk, the provider may recommend additional screening technologies to get a more accurate view (See Other Screening Tests).
For women who undergo a standard mammogram, 2 views of each breast must be captured, and this can cause some temporary discomfort for women as the breasts are placed in a position to capture these images, but this discomfort dissipates quickly, Rhodes says. The radiology facility that conducts the test and reads the results is required by federal law to send a letter detailing if the mammogram is normal, negative, or if there is an abnormality that requires further evaluation. Rhodes says women can follow up with the radiologist to ask questions or get more information about the results.
“The radiologist is the best person to speak with about your mammogram,” states Rhodes. “Often the primary care provider who ordered the test is not in the best position to advise you what to do, because they didn’t interpret the test and/or the provider is not the expert in all of the nuances of interpreting the mammogram. The radiologist is a great resource for questions about the findings on the mammogram and the options for screening in the future.”
Rhodes reminds all women that the idea of screening is to get ahead of cancer, minimize treatment side effects, and provide an optimal outcome. “The goal of screening is to detect cancer as early as we can, so we can treat it less invasively and have a better likelihood of curing it.”